
e102
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
with pancreatic mass and biliary stent are lacking. The aim of this
study is to evaluate the influence of biliary stent on the adequacy
and accuracy of EUS-FNTA performed with fenestrated needles in
patients with pancreatic head masses.
Material and methods:
All patients who underwent EUS-FNTA
with fenestrated needles of solid pancreatic head masses causing
obstructive jaundice in a single centre from January 2013 to January
2015, were retrospectively identified. The primary outcome measure
was the adequacy, defined as the rate of cases in which a tissue
specimen for histological examination was achieved. Secondary
outcome measures were the accuracy, defined as the proportion of
correct diagnoses made with and without stent and the complication
rate. Standard references were the surgical specimen when available
or other diagnostic investigations together with long-term follow-
up (>6 months).
Results:
A total of 109 patients with pancreatic head mass causing
biliary obstruction were included in the study: 56 cases of them
were sampled without stent and 53 cases with stent in situ (all
plastic stents). The adequacy was 96.2% in the stent group and
91.1% in the group without stent (p=0.582). Final diagnosis was:
103 (94.5%) cases of adenocarcinoma, 4 focal pancreatitis (3.5%),
1 neuroendocrine carcinoma (1%) and 1 metastasis (1%). No
significant differences were observed for sensitivity (88.2% vs.
83.3%), specificity (100% for both groups), and accuracy (88.7% vs.
83.9%) between those with and without stent, respectively. False
negative results were encountered in 6/53 (11.3%) cases with stent
vs. 9/56 (16%) cases without stent. The accuracy was not influenced
by the timing of stenting (<48 hours or ≥48 hours before EUS). No
EUS-FNTA related complications were recorded.
Conclusions:
The presence of plastic biliary stent does not influence
the tissue sampling adequacy and the diagnostic accuracy of EUS-
FNTA of pancreatic head mass performed with fenestrated needles.
OC.08.8
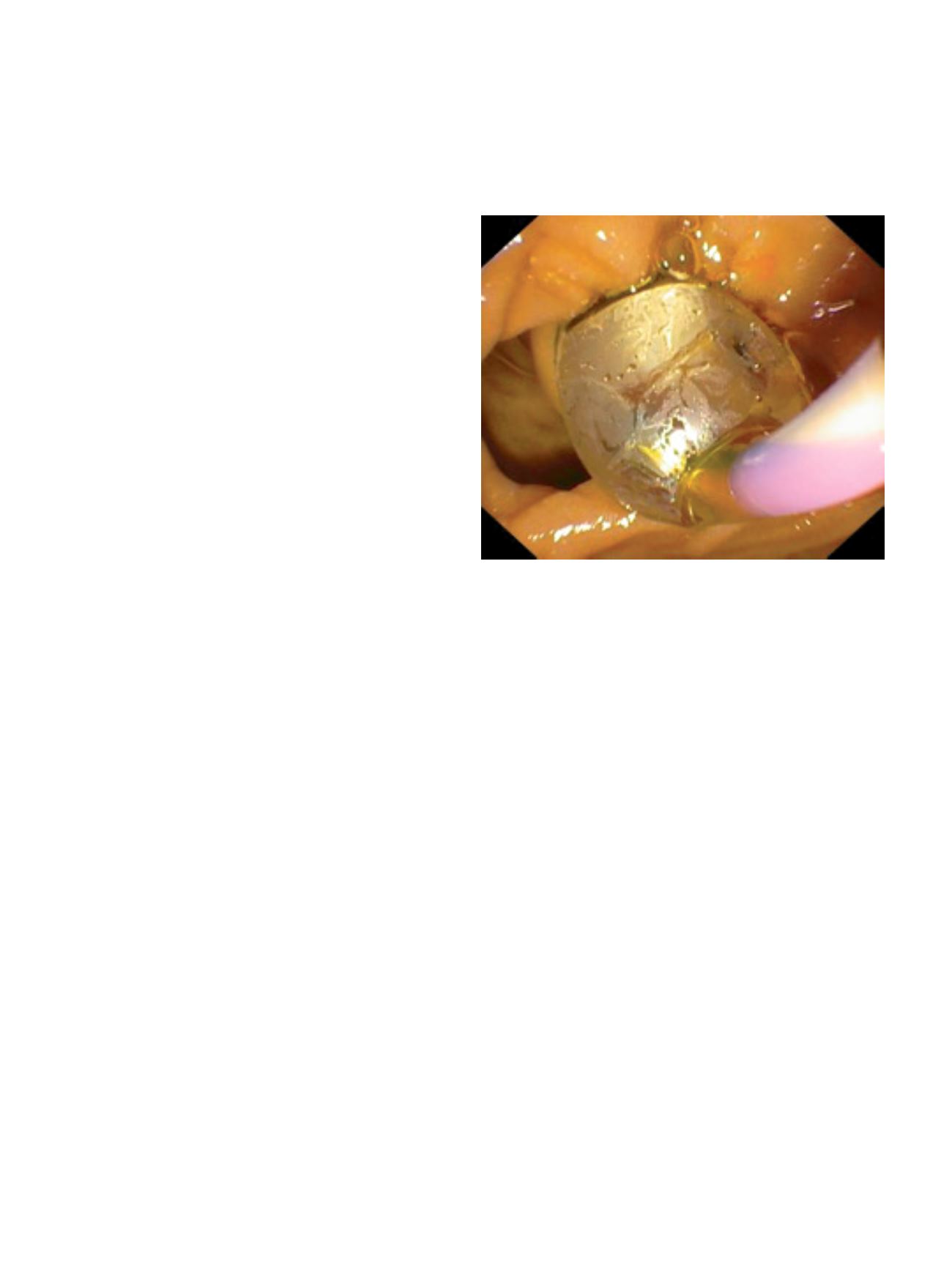
ENDOSCOPIC PAPILLARY LARGE BALLOON DILATION FOR LARGE
STONES EXTRACTION IN PATIENTS WITH PERI-AMPULLARY
DIVERTICULA
Zulli C.*, Gargiulo L., Labianca O., Quagliariello G., Riccio G.,
Tammaro S., Maurano A.
University Hospital San Giovanni di Dio e Ruggi d’Aragona, Ospedale
Amico G. Fucito, Mercato San Severino, Salerno, Italy
Background and aim:
Dilation Assisted Stone Extraction [DASE] has
been proposed as an alternative technique to simple ES for extraction
of large common bile duct [CBD] stones extraction (≥ 10 mm). Peri-
ampullary diverticula [PAD] can be divided in type 1 (papilla inside
the diverticulum), type 2 (papilla on the margin) and type 3 (papilla
outside). The presence of PAD is a technical difficulty for stones
removal and can cause more complications. We aimed to evaluate
the efficacy and safety of DASE for large CBD stone extraction in
patients with PAD.
Material and methods:
A retrospective analysis of 42 DASE
procedures in patients with PAD and large CBD stones was
effectuated.
Results:
Median age of patients was 75 years, 17 were males and 25
females. About 17% of patients had a type 1 PAD, 33% type 2 and 50%
type 3. About 48% of patients had a single large stone. Stones were
mainly located in CBD. Mean size of stones was 13.9±4.32mm. A
precut sphincterotomy was effectuated in 4/42 patients. Cannulation
rate was 95.2% (40/42). Wirsung was cannulated in 28% of
procedures. Stone extraction success was reached 91% (41/45). ML
was performed in two cases and use of Dormia was avoided in 38%
of cases. Spontaneous stones expulsion occurred in 28% of cases.
Pancreatic plastic stent was placed in two patients. Endoscopic
evidence of mild self-limiting bleeding, without clinical support,
occurred in 4 patients (9.5%). Only one patient had a clinical evidence
of mild bleeding (Hb drop 1.5 g/dL without need for transfusion).
One patient had a mild pancreatitis after procedure. No severe or
fatal outcomes were observed. No differences in complications rate
were observed with respect to Indometacine use. No differences
were observed in procedure results regarding papilla location with
respect to the diverticula and dilation time (30” or 60”).
Conclusions:
This is one of the first studies evaluating efficacy and
safety of DASE for CBD large stones extraction in patients with PAD.
Despite the small number of patients, this technique seems to be
safe and effective in patients with PAD, independently of papilla
location.
OC.08.9
IMPLEMENTING SPLIT REGIMEN OVER SINGLE DOSE (IMPROVES):
A QUALITY IMPROVEMENT (QI) PROJECT TO IMPROVING BOWEL
PREPARATION IN CLINICAL PRACTICE. PRELIMINARY RESULTS
FROM SIED CAMPANIA NETWORK
De Bellis M.*
10,
Rotondano G.
1
, Di Giulio E.
2
, Maxemiliano G.
3
,
Grasso E.
4
, Hassan C.
5
, Labianca O.
6
, Scaffidi M.
7
, Tarantino O.
8
,
Galloro G.
9
and SIED Campania IMPROVES study group.
1
Gastroenterology and Digestive Endoscopy Unit, ASL NA 3 Sud - A.
Maresca Hospital, Torre del Greco (NA), Italy,
2
Gastroenterology and
Digestive Endoscopy Unit, Sant’Andrea Hospital, Sapienza University,
Rome, Italy,
3
Gastroenterology and Digestive Endoscopy Unit, Santa
Maria della Misericordia Hospital, Urbino, Italy,
4
Gastroenterology
Unit, Tor Vergata University, Rome, Italy,
5
Gastroenterology Unit,
Nuovo Regina Margherita Hospital, Rome, Italy,
6
AOIU San Giovanni di
Dio e Ruggi d’Aragona - Gaetano Fucito Hospital - Digestive Endoscopy
Unit, Mercato San Severino (SA), Italy,
7
Gastroenterology and Digestive
Endoscopy Unit, Santa Maria della Stella Hospital, Orvieto (TR), Italy,
8
Gastroenterology and Digestive Endoscopy Unit, Nuovo San Giuseppe
Hospital, Empoli (FI), Italy,
9
Surgical Endoscopy Unit, Department of
Clinical Medicine and Surgery, Federico II University, Naples, Italy,
10
Endoscopy Unit, National Cancer Institute and G. Pascale Foundation
IRCCS, Naples, Italy
Background and aim:
Bowel preparation affects the quality and
value of colonoscopy. Split-dosing is considered a key measure for
improving bowel preparation. Despite ESGE guideline recommends
all patients receiving split-dose, the reporting rates of split regimen
are still too low in the real world.


















