
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e101
technical failure: 1 FAP (4.6%), 5 SAA (13.5%). 6 patients were lost to
follow up.
Histology showed: nonspecific changes (8.5%), low grade dysplasia
(37.3%), high grade dysplasia (39%) and carcinoma (11.9%). No
carcinoma in the FAP group.
Biopsy sampling accuracy was higher for low grade dysplasia (77.3%)
compared with high grade dysplasia (17.4%) or carcinoma (14.3%) in
both group.
Conclusions:
Endoscopic papillectomy of selected ampullary
tumors is a safe and effective procedure and, as it can achieve a
complete endoscopic resection, it should be established as the first
line therapy of ampullary adenomas.
OC.08.5
HAVE INTRAVENOUS PROTON PUMP INHIBITORS BETTER
CLINICAL OUTCOME RESPECT TO ORAL PPI IN PATIENTS WITH
PEPTIC ULCER BLEEDING: A META-ANALYSIS
Tringali A.*, Sica M., Manta R., Mutignani M.
Ospedale Niguarda, Milano, Italy
Background and aim:
The efficacy of Proton pump inhibitors (PPI)
has been proved in peptic ulcer bleeding but the administration
route remain controversial. Several studies have shown that oral
PPI at high dose is effective as intravenous PPI in reducing recurrent
bleeding. However current guideline recommend to use intravenous
PPI after endoscopic treatment. To the best of our knowledge a
previous metanalysis showed that oral and IV PPI have similar
clinical effectiveness but the conclusion was limited by insufficient
sample size. To compare the oral and intravenous PPI in patients
with peptic ulcer bleeding a metanalysis was performed.
Material and methods:
A computerized medical literature search
was performed by using MEDLINE, EMBASE, Cochrane Library, from
1980 to March 2015 aimed at identifying available studies that
assess efficacy of different route of administrtion of PPI. We finally
analyzed 9 RCTS, involving 1021 patients.
Outcomes were: rebleeding rate, blood transfsion requirement,
hospital stay, surgery and mortality.
Results:
There was no difference in rebleeding rate (OR 0.94 85%CI
0.62-1.42) and mortality (OR 0.57, 95%CI 0.22-1.49). Of note surgery
and need for blood transfusion were higher in iv PPI group (OR 0.32,
95%CI 012-0.90; SMD-0.5795%CI -0.89,-00.25), while hospital stay
(SMD -0.73 95%CI -1.70, 0.24) and mortality were equivalent (OR
0.57 95%CI0.22-1.49).
Conclusions:
Intravenous PPI is not superior to oral PPI. Oral PPI
seems to have less need for surgery and blood transfusion. More
RCTs are warranted to clarify this results.
OC.08.6
EVALUATION OF A NEW THERAPEUTIC LASER SYSTEM
FOR ENDOSCOPIC SUBMUCOSAL DISSECTION (ESD) IN AN
ESTABLISHED ANIMAL MODEL
Tontini G.E.*
1
, Neumann H.
2
, Carmignani L.
5
, Bruni B.
3
, Soriani P.
1
,
Cavallaro F.
1
, Fagnani F.
4
, Clemente C.
3
, Bottani M.
1
, Vecchi M.
1
1
Gastroenterology & Digestive Endoscopy Unit, IRCCS Policlinico San
Donato, San Donato Milanese, Milano, Italy,
2
Department of Medicine
I, University of Erlangen-Nuremberg, Erlangen, Germany,
3
Pathology
and Citodiagnostic Unit, IRCCS Policlinico San Donato, San Donato
Milanese, Milan, Italy,
4
Surgical Division, Quanta System SpA, Varese,
Italy,
5
Academic Urology Department, IRCCS Policlinico San Donato,
San Donato Milanese, Milano, Italy
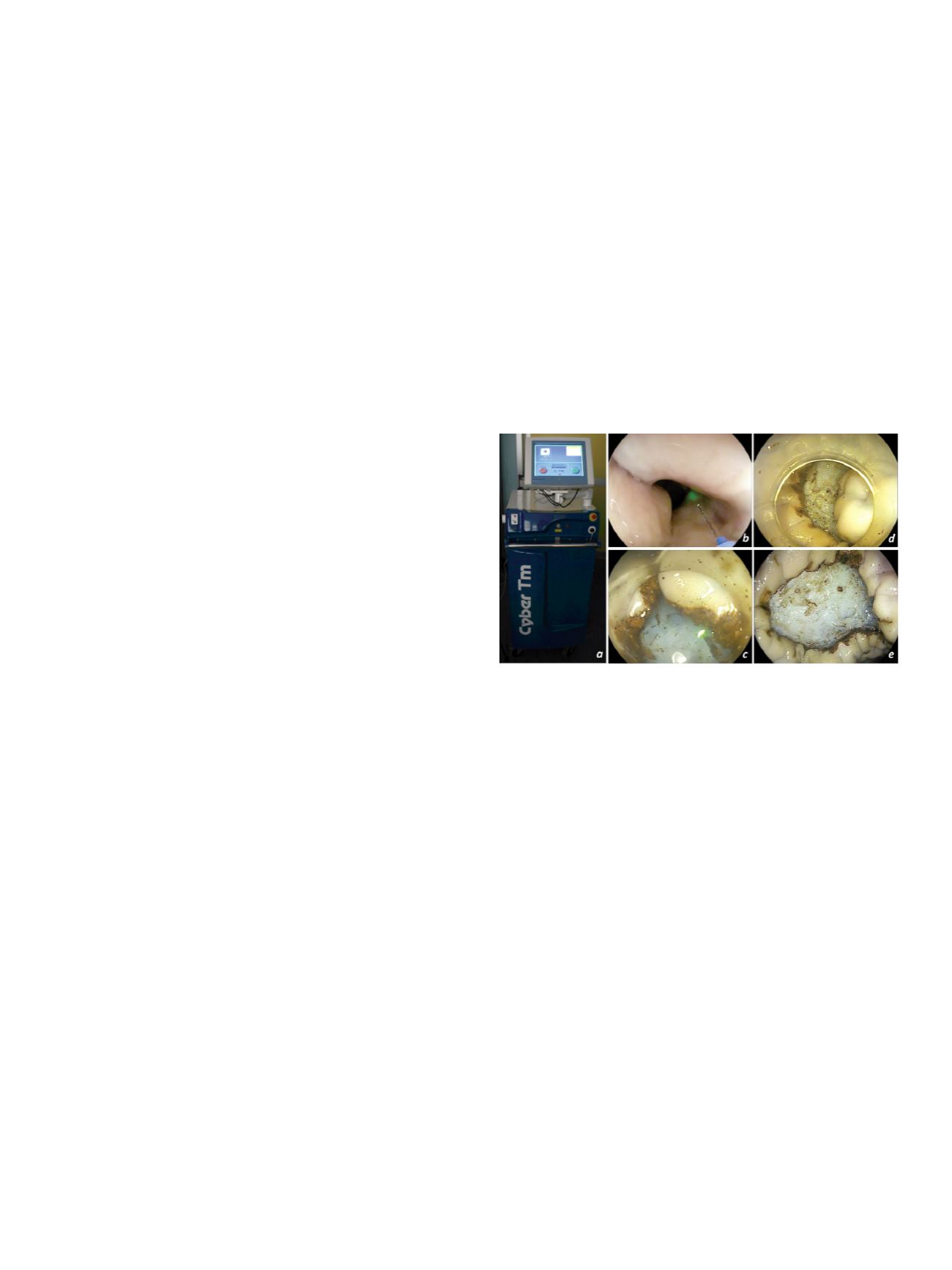
Background and aim:
The Thulium laser system is a novel
therapeutic technique for open surgery and endourological
treatments [1,2] (fig. a). To date, the experience on the use of the
Thulium laser system in gastrointestinal (GI) endoscopy is very
limited [3].
Material and methods:
We conducted the first pilot study in an
established experimental setting by using the EASIE model to test
the feasibility and safety of the newly introduced Thulium laser
system (Cyber TM®, Quanta System, Varese, Italy) for endoscopic
submucosal dissection (ESD) in GI endoscopy. Therefore, different
optical fibers suitable for digestive endoscopy (272 and 365 um
thick), were evaluatedwith various power settings (15, 20, 25, 30, and
35 watts), and laser configurations (continued laser shaping or pulse
modality). The ESD procedure of artificial lesions of the stomach was
performed in standard technique and digitally recorded. An expert
GI pathologist performed histopathological analysis.
Results:
Neither transmural perforation, nor any muscular layer
damagewas observed. Both the fiber diameters and the configuration
modalities (continued or pulse modality) were safe, effective, and
precise. R0 resection was feasible in all cases. A complete ESD of a 35
mm lesion by using the new Thulium Laser system took
approximately 70 minutes (fig. b-e). In addition, a fast learning
curve was involved.
Conclusions:
The new Thulium laser system appears to be an
effective technique for ESD in upper GI endoscopy. This novel
therapeutic technique for gastrointestinal endoscopy has also
shown a high level of precision and safety in an ex vivo animal
model. In vivo studies are now highly warranted to confirm these
initial results.
References:
1. Rieken M & Bachmann. Nat Rev Urol 2014.
2. Carmignani L, et al. Asian J Androl 2015.
3. Cho JH, et al. Endoscopy 2013.
OC.08.7
BILIARY STENT DOES NOT INFLUENCE THE ADEQUACY AND
ACCURACY OF EUS-GUIDED TISSUE ACQUISITION WITH
FENESTRATED NEEDLES OF PANCREATIC MASSES CAUSING
OBSTRUCTIVE JAUNDICE
Antonini F.*
1
, Fuccio L.
2
, Fabbri C.
3
, Frazzoni L.
2
, Belfiori V.
1
,
De Minicis S.
1
, Lo Cascio M.
1
, Marraccini B.
1
, Piergallini S.
1
,
Andrenacci E.
1
, Macarri G.
1
1
Ospedale A.Murri, Fermo, Italy,
2
Ospedale Sant’orsola, Bologna, Italy,
3
Ospedale Bellaria-Maggiore, Bologna, Italy
Background and aim:
Patients with pancreatic masses causing
obstructive jaundice candidates to endoscopic ultrasound (EUS) for
the diagnosis and staging and to ERCP for stenting, should perform
EUS first. However, it is not infrequent to perform EUS when
biliary stent is already in situ. While the presence of biliary stent
significantly decrease the accuracy of EUS for pancreatic head cancer
staging, its impact on the EUS-guided tissue sampling adequacy
and accuracy is still debated. Furthermore, data on EUS-fine needle
tissue acquisition (EUS-FNTA) with fenestrated needles in patients


















