
e96
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
Conclusions:
IBS overlaps more frequently with FH than with
GERD, suggesting common pathways and treatment for these two
functional GI disorders. The nomograms derived from the ISAC and
the ISAA-HH predictive models allow a high level of suspicion for FH
and can be useful in clinical practice.
OC.07.3
RECOVERY OF GASTRIC FUNCTION AFTER ACETIUM®
ADMINISTRATION: A 2 YEAR PROSPECTIVE STUDY IN PATIENTS
WITH CHRONIC, ATROPHIC, BODY GASTRITIS
Di Mario F.*
1
, Ricco’ M.
4
, Dal Bo’ N.
2
, Ferrara F.
2
, Marcello R.
2
,
Grande G.
1
, Franceschi M.
3
, Scarpignato C.
1
, Rugge M.
5
1
Department of Clinical and Experimental Medicine, University of
Parma, Parma, Parma, Italy,
2
Gastroenterology and Gastrointestinal
Endoscopy Unit, Treviso Hospital, Treviso, Italy,
3
Endoscopic Unit
- Department of Surgery, ULSS 4 AltoVicentino, Santorso, Vicenza,
Italy,
4
Dipartimento di Prevenzione, Unità Operativa di Prevenzione e
Sicurezza degli Ambienti di Lavoro, Azienda Provinciale per i Servizi
Sanitari della Provincia Autonoma di Trento, Trento, Italy,
5
Department
of Pathology, University of Padua, Padua, Italy
Background and aim:
The relationship between H.pylori eradication
and atrophic changes in the gastric mucosa has not yet been fully
elucidated. Although some studies report a partial restoration of
pepsinogen I (PGI) levels after eradication, it is not clear whether
this finding reflects gastric healing. L-cysteine (Acetium(TM), Biohit
Oyj, Finland), an agent capable of reducing acetaldehyde after food
intake, has been proposed for prevention of gastric carcinogenesis in
patients with body CAG. Present study aims to assess modifications
in gastric function after Acetium(TM) administration in body CAG by
means of PGI, PGII and G-17 serum levels.
Material and methods:
65 patients (M:F=19:46, mean age 52.2±9.3
years), with histological diagnosis of body CAG (according to the
O.L.G.A. staging) and PGI < 25 µg/L, underwent upper GI endoscopy
with gastric biopsy samplings and PGI, PGII and G-17 by means of
Gastropanel(R) (Biohit Oyj, Helsinki, Finland). Among the patients,
26 had autoimmune gastritis while 39 of them reported previous
H.pylorii infection. All the patients were treated with AcetiumTM
(100 mg three times daily) for 24 months. PGI, PGII and G-17 values
were measured at baseline and at T+3, T+6, T+12, T+18 and T+24
months and confronted through a General Linear Model adapted for
repeated measures.
Results:
PGI and PGII values did not significantly differ at the end
of follow up (in both cases, GLM p value > 0.05), and covariates
such as age, baseline disorders and sex were not associated with
a significantly different effect. On the other hand, G-17 values
significantly decreased during the follow-up (p = 0.018), in particular
after the first year of treatment (46.1±36.9 pmol/L at baseline vs
34.7±28.2 pmol/L at T+12 months, and 28.1±19.8 at T+24). Subjects
of male sex (p = 0.022) and post-H.pylorii infection status (p = 0.034)
presented the most significant reduction of G-17 values.
Conclusions:
After Acetium(TM) administration, patients with
body CAG showed improvements of gastric function, reflected by
a significant decrease of G-17, with a more evident effect on male
subjects and in cases with a previous diagnosis of H. pylori infection.
As the reduction of G-17 serological values is more evident after 12
months of treatment, it should not be discontinued even after initial
clinically unsatisfying results.
OC.07.4
GASTROESOPHAGEAL REFLUX DISEASE BEFORE AND AFTER
LAPAROSCOPIC SLEEVE GASTRECTOMY: LONG TERM RESULTS
Santonicola A.*
1
, Ciacci C.
1
, Angrisani L.
2
, Iovino P.
1
1
Gastrointestinal Unit, Department of Medicine and Surgery,
University of Salerno, Salerno, Italy,
2
General and Endoscopic Surgery
Unit, S. Giovanni Bosco Hospital, Naples, Italy
Background and aim:
Laparoscopic Sleeve Gastrectomy (LSG) is
becoming the most performed bariatric procedure, however, data
available on long-term follow-up are scanty. The effects of LSG on
GERD remain controversial. Objectives: Evaluate the 5 years efficacy
of LSG on weight loss and gastroesophageal reflux disease (GERD)
symptoms.
Material and methods:
105 obese patients eligible for bariatric
surgery underwent LSG. According to the preoperative Body Mass
Index (BMI) obese patients were divided in two Groups: Group 1
(N=61, patients with preoperative BMI ≤ 50 Kg/m2) and Group 2
(N=44, patients with preoperative BMI > 50 Kg/m2). All underwent
a preoperative assessment including evaluation of comorbidities,
standardized GERD questionnaire, a double-contrast barium
swallow (dc-BS), an upper-gastrointestinal endoscopy (UGIE). The
postoperative evaluation was performed at at 1, 3, 5 year after
surgery. At each follow-up visit the following data were collected:
weight (expressed as BMI, Delta BMI [BMI at follow-up - preoperative
BMI], Total Weight Loss[%TWL]), and GERD symptoms.
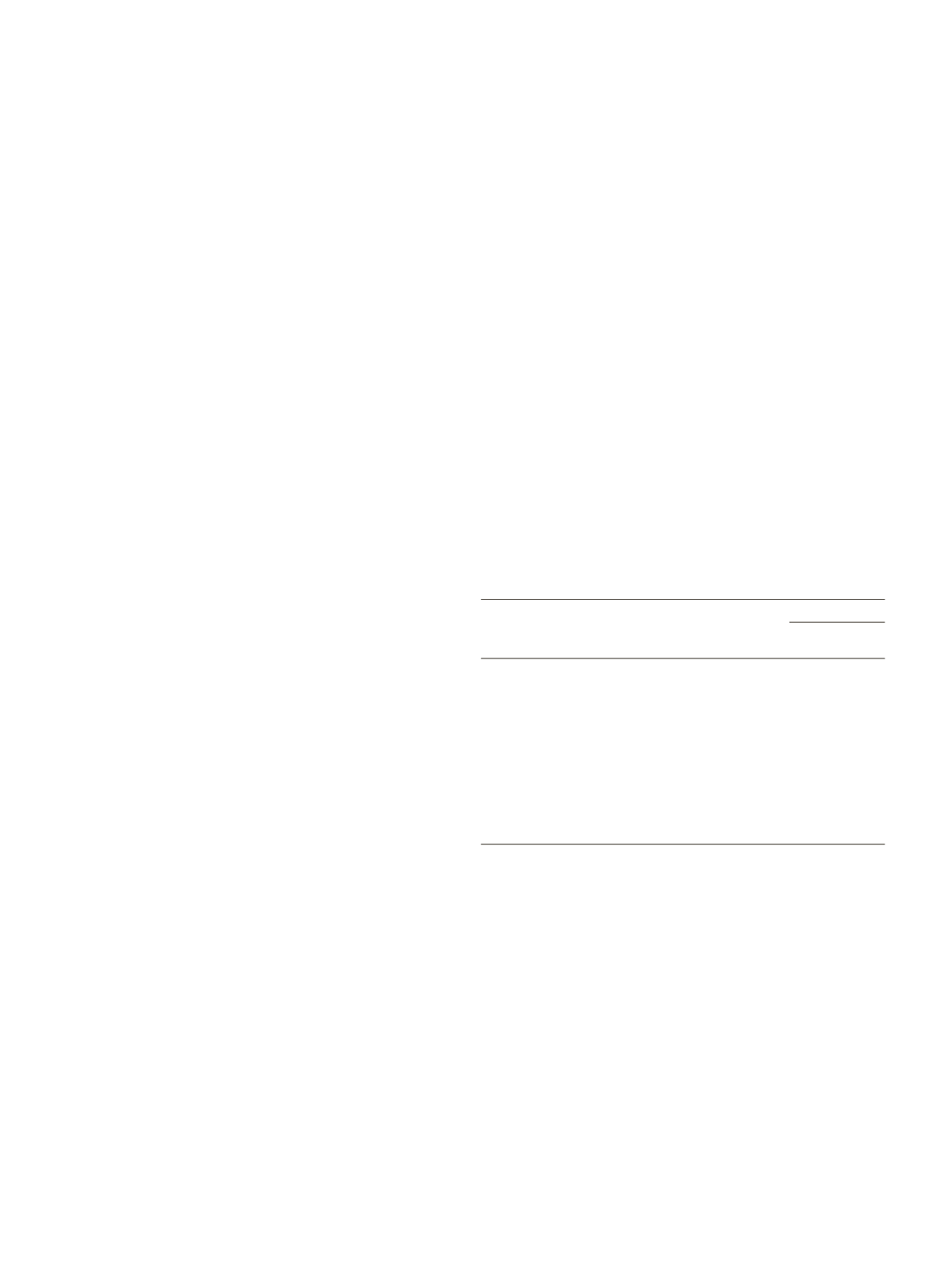
Table 1
Linear regression model with the TWL% as dependent variables, and age, gender,
post-operative prevalence of GERD, T2DM, hypertension and hyperlipidemia as
covariates
Confidence interval
Lower
Upper
Parameter
B
SE
t
Sig
limit
limit
Intercept
51.65
6.07
8.51
0.000 39.57 63.72
Age
-0.43
0.11
-3.89 0.000 -0.65
-0.21
Gender
0.41
2.34
0.18
0.86
-4.23
5.06
Postoperative
-6.26
2.80
-2.24
0.03
-11.83 -0.70
GERD
Postoperative
5.62
7.81
0.72
0.47
-9.93
21.16
T2DM
Postoperative 0.026
3.33
-1.18
0.24
-10.38
2.64
Hypertension
Postoperative
-3.86
3.27
-1.18
0.24
-10.37
2.64
Hyperlipidemia
*SE=Standard Error
Results:
BMI at surgery was 41±5 Kg/m2 in Group1 vs 57±6 Kg/m2
in Group2 (p<0.001). Age at surgery was similar in the two Groups
(p=0.5). 31% of Group1 vs 25% of Group2 referred preoperative GERD
symptoms (p=0.6). In 16% of patients of Group1 and 7% of Group2
the preoperative dc-BS and/or the UGIE revealed the presence of
hiatal hernia (HH). Patients with typical GERD symptoms showed a
significantly higher prevalence of HH compared to patients without
GERD complains (23.1% vs. 6.8%, p=0.02). At 5 years of follow-up,
the BMI was 30.1± 4.8 Kg/m2 in Group 1 vs 37.8± 8.3 Kg/m2 in
Group 2(p<0.001). Delta BMI was significantly higher in Group 2
than in Group 1 at 1-3 and 5 years (p<0.001). Group 2 showed also
a significantly higher %TWL (26.6±18.3 vs 33.5±12.9, p=0.006) than
Group 1. No significative differences were found in postoperative
typical GERD symptoms between Group 1 and Group 2 patients
(18.2% vs 20%, p=0.83). Among the patients of Group 1: 65% referred
the resolution, 35% the persistence and 15% the new onset of
GERD complaints. Among the patients of Group 2, 44% referred
the resolution, 56% the persistence and 8% the new onset of GERD
complaints. Younger age at surgery and absence of postoperative


















