
e94
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
Background and aim:
A nonresponse to ursodeoxycholic acid
(UDCA) is significantly more common in primary biliary cirrhosis
(PBC) patients who are diagnosed before age 50 or who are male.
Patients with a non-response to UDCA are at significantly increased
risk of an adverse outcome such as end-stage liver disease or
liver transplantation [1,2]. Obeticholic acid (OCA), a potent and
selective farnesoid X receptor (FXR) agonist, induced significant
liver biochemistry improvements in 3 randomized, placebo (PBO)-
controlled trials in PBC patients both as a monotherapy or in
combination with UDCA. This integrated analysis evaluates the
efficacy and safety of OCA in PBC subpopulations based on age and
sex.
Material and methods:
Data were pooled across the 3 trials and
endpoints were based on end of double-blind (DB) treatment.
Treatment arms: PBO (n=134) and OCA ≤10 mg (n=201). Efficacy
endpoints were the LS mean change from baseline (BL) in ALP and
a composite endpoint (% of patients achieving an ALP <1.67x ULN,
total bilirubin ≤ULN and an ALP decrease ≥15% from BL). Increased
serum ALP and bilirubin levels have been strongly associated with
reduced transplant-free survival. Safety and tolerability were also
assessed.
Results:
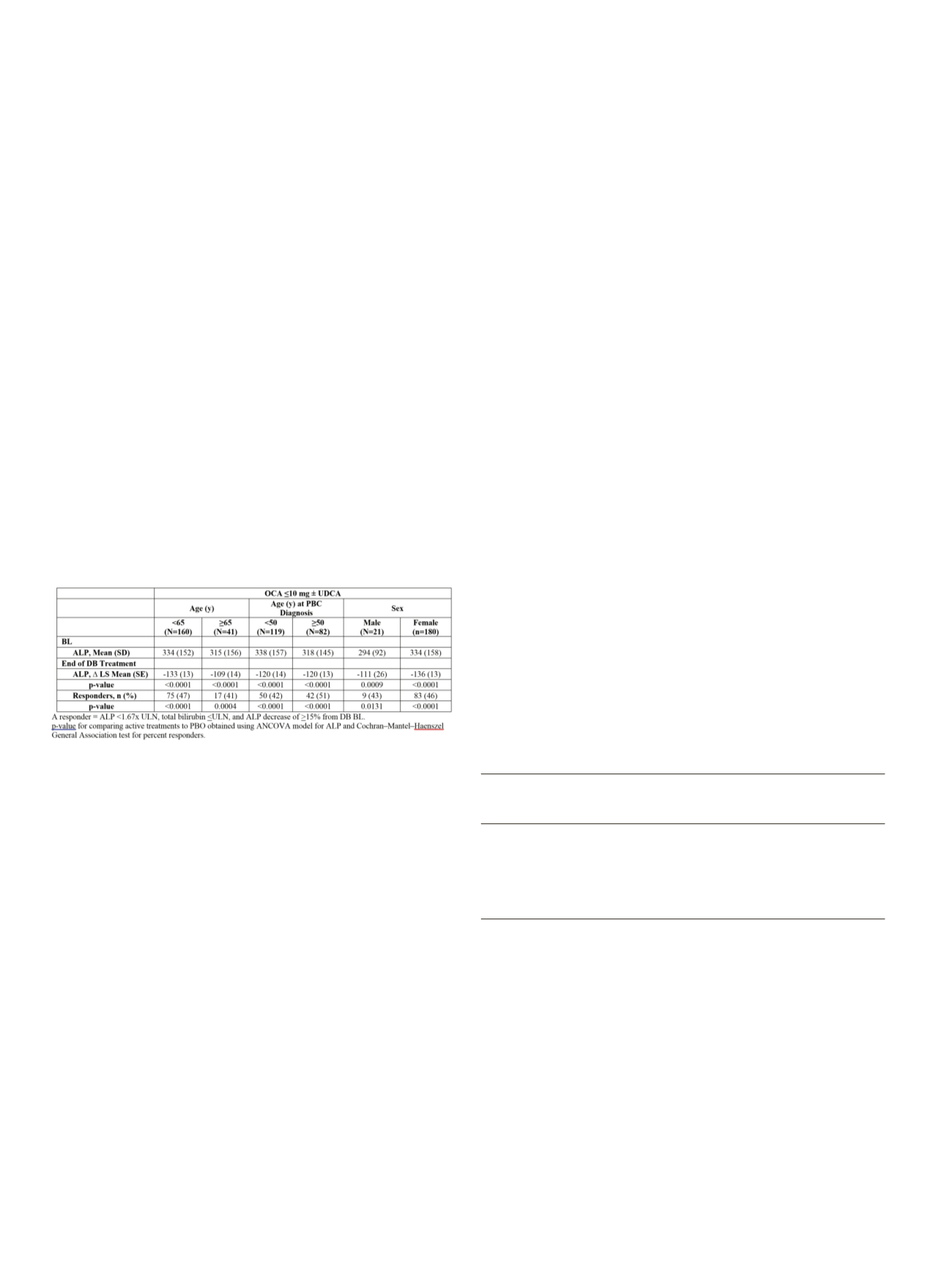
Irrespective of age, age at PBC diagnosis, or sex, OCA ≤10 mg
treatment resulted in significant decreases in ALP and a higher
percentage of patients achieving the composite endpoint, compared
with PBO (Table). Safety and tolerability were similar across age and
gender subgroups. Pruritus was the most frequently occurring TEAE
regardless of subgroup. Incidence of pruritus was 63 vs 51% for
<65/≥65 y, 62 vs 57% for age at PBC diagnosis<50/≥50 y, and 57 vs
61% for male/female subgroups.
Conclusions:
In contrast to PBO, significant improvements in ALP,
highly predictive of outcomes, were observed across age and sex
subgroups with OCA ≤10 mg. This is clinically relevant as younger
patients and males who do not respond to UDCA are at higher risk of
adverse outcomes/poor prognosis. OCA was generally safe and well
tolerated.
References
1. Lammers WJ et al. Gastroenterology (2015), doi: 0.1053/j.gastro.2015.07.061
2. Carbone M et al. Hepatology (2015), doi: 10.1002/hep.28017
OC.06.9
IRRITABLE BOWEL SYNDROME: RESULTS OF AIGO SURVEY 2014-
2015
Soncini M.*
1
, Milazzo G.
8
, Leandro G.
2
, Bellini M.
3
, Carrara M.
4
,
Montalbano L.
5
, Muscatiello N.
6
, Monica F.
7
, Usai Satta P.
9
, Cabras F.
9
,
Camilleri S.
10
, Gambaccini D.
3
, Tammaro L.
11
, D’Alba L.
11
, Turco L.
12
,
Gasparini P.
1
, Galeazzi F.
13
, Solinas A.
14
, Russo G.
15
, Salvioli B.
16
,
Anderloni A.
16
, Bassotti G.
17
, Lai M.
18
, Antonino M.
6
, De Bona M.
19
,
Boschetto S.
20
, Rentini S.
21
, Rossitti P.
22
, Limido E.
23
, Balzano A.
24
1
A.O. San Carlo Borromeo, Milano, Italy,
2
IRCCS S. de Bellis, Castellana
Grotte (BA), Italy,
3
A.O. Università Pisana, Pisa, Italy,
4
Ospedale
Orlandi, Bussolengo (VR), Italy,
5
Ospedali Riuniti Villa Sofia-Cervello,
Palermo, Italy,
6
Ospedali Riuniti di Foggia, Foggia, Italy,
7
Ospedale
di Cattinara, Trieste, Italy,
8
Ospedale Vittorio Emanuele III, Salemi
(TP), Italy,
9
Azienda Ospedale Brotzu, Cagliari, Italy,
10
Ospedale
San Cataldo, Caltanissetta, Italy,
11
A.O. San Giovanni Addolorata,
Roma, Italy,
12
Ospedale Copertino, Lecce, Italy,
13
Azienda Ospedaliera
Padova, Padova, Italy,
14
USL Umbria 1, Perugia, Italy,
15
Ospedale San
Andrea, La Spezia, Italy,
16
IRCCS Humanitas Rozzano, Milano, Italy,
17
IRCCS Perugia, Perugia, Italy,
18
Ospedale Monserrato, Cagliari, Italy,
19
Ospedale di Feltre, Belluno, Italy,
20
Ospedale Rieti, Rieti, Italy,
21
A.O.
Universitaria Senese, Siena, Italy,
22
A.O. S. Maria della Misericordia,
Udine, Italy,
23
A.O. S. Anna - P.O. Cantù, Como, Italy,
24
Napoli, Napoli,
Italy
Background and aim:
to determine the quality of life of patients
(pts) who refer to Italian outpatient Gastroenterology clinics with
a known or a first diagnosis of irritable bowel syndrome (IBS)
according to Rome III criteria. Secondary aim: to determine whether
the distribution of diagnostic resources can be appropriate.
Material and methods:
Data from 26 AIGO centres on outpatients
affected by IBS, according to Rome III criteria, have been prospectively
collected from 1st July 2014 to 30st June 2015. Patients were asked to
fill in an anonymous format the following questionnaires: Hospital
Anxiety and Depression Scale (HADS), the Short Form (SF12) and
the Irritable Bowel Syndrome Severity Scoring System (IBS-SSS).
Data on medical care during the course of the previous year were
also recorded: number of visits by the general practitioner and
gastroenterologist, diagnostic tests, working days lost.
Results:
683 records on IBS pts (mean age 43.1 ± 15.2 yrs, 73% F,
27% M) were collected. 51.2% of the patients were a first diagnosis.
Using a visual analogue scale (VAS) (0-100 mm), abdominal
pain severity had a mean value of 47.1±23.3, abdominal bloating
53.0±24.4, presence of abdominal pain on a 10 days period 5.2 ±
3.0; satisfaction for bowel habit 28.8±22.9; change in their habits of
living and working 47.7±25.7. According to the questionnaire HADS
Anxiety, 35.8% had a score greater than 11; according to the HADS
Depression, 14.5% had a pathological score (>11). Pts with a first
diagnosis of IBS were significantly younger in respect to pts with a
known diagnosis, 40.2±14.8 vs 46.1±15.1 (p<0.001) respectively, but
did not differ for all other variables included in IBS-SSS and HADS.
Data on medical care during the course of the previous year were
reported in table 1.
Table 1
Procedures in IBS patients
350 patients
333 patients
with 1th diagnosis
with known diagnosis
Procedure
N
of IBS (%)
of IBS (%)
MRI
11
6 (1.7)
5 (1.5)
US abdomen 444
202 (57.7)
242 (72.6)
CT abdomen
33
9 (2.5)
24 (7.2)
Sigmoidoscopy
20
9 (2.5)
11 (3.3)
Colonscopy
363
147 (42.0)
216 (64.8)
MRI = Magnetic Resonance Imaging ; US = Ultrasound
Conclusions:
Data from this survey conducted in the AIGO Italian
gastroenterology clinics demonstrated the high degree of disability
of pts with IBS that is maintained over the time. The lack of
difference between old and new diagnosed IBS shows that current
treatments are largely unsatisfying. The use in a large number of pts
of invasive procedures, such as colonoscopy, indicates a widespread
inappropriateness.


















