
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e89
to those observed in patients with GERD. In a relevant percentage of
NOD patients, a pathological acid exposure in the distal esophagus
might sensitize esophageal mucosa to an increased perception of
esophageal bolus passage, and, therefore might explain dysphagia
occurrence.
OC.05.6
CLINICAL CHARACTERISTICS AND OUTCOMES OF POEM
ACCORDING TO ACHALASIA MANOMETRIC PATTERN. DO
THE OUTCOMES OF TREATMENT DEPEND ON MANOMETRIC
SUBTYPE?
Cali’ A.*, Familiari P., Gigante G., Landi R., Boskoski I., Tringali A.,
Barbaro F., Andrade Zurita S., Perri V., Costamagna G.
Fondazione Policlinico Universitario A. Gemelli, Roma, Italy
Background and aim:
According to High Resolution Manometry
(HRM), achalasia can be classified into 3 types. Previous studies on
pneumatic dilation and surgical myotomy demonstrated that worst
outcomes are associated with the type III. One of the theoretical
benefits of Per-Oral Endoscopy Myotomy (POEM) is that the length
of myotomy can be customized according to the HRM findings. Aim
of this study is to investigate characteristics and POEM outcomes of
3 achalasia types in a large series of patients.
Material andmethods:
A total of 290 patients with achalasia treated
with POEM between 2011 and October 2015, were retrospectively
identified on a prospective database. Patients who underwent HRM
during preoperative work-up, and with a minimal 6 months follow-
up were enrolled.
POEM was performed according to the Inoue’s technique. In case of
type I and type II achalasia an 8-12 cm myotomy was performed.
In case of type III achalasia myotomy was usually longer (>12cm).
ANOVA and Pearson Chi-square test were used to find associations
between achalasia types with baseline characteristic (age, gender,
Eckardt score, symptoms duration, previous treatments, esophageal
shape, diameter and LES pressure), procedure time and POEM
outcomes (ECK<4). If there was a statistically significant difference a
post hoc analysis was performed using LSD method.
Results:
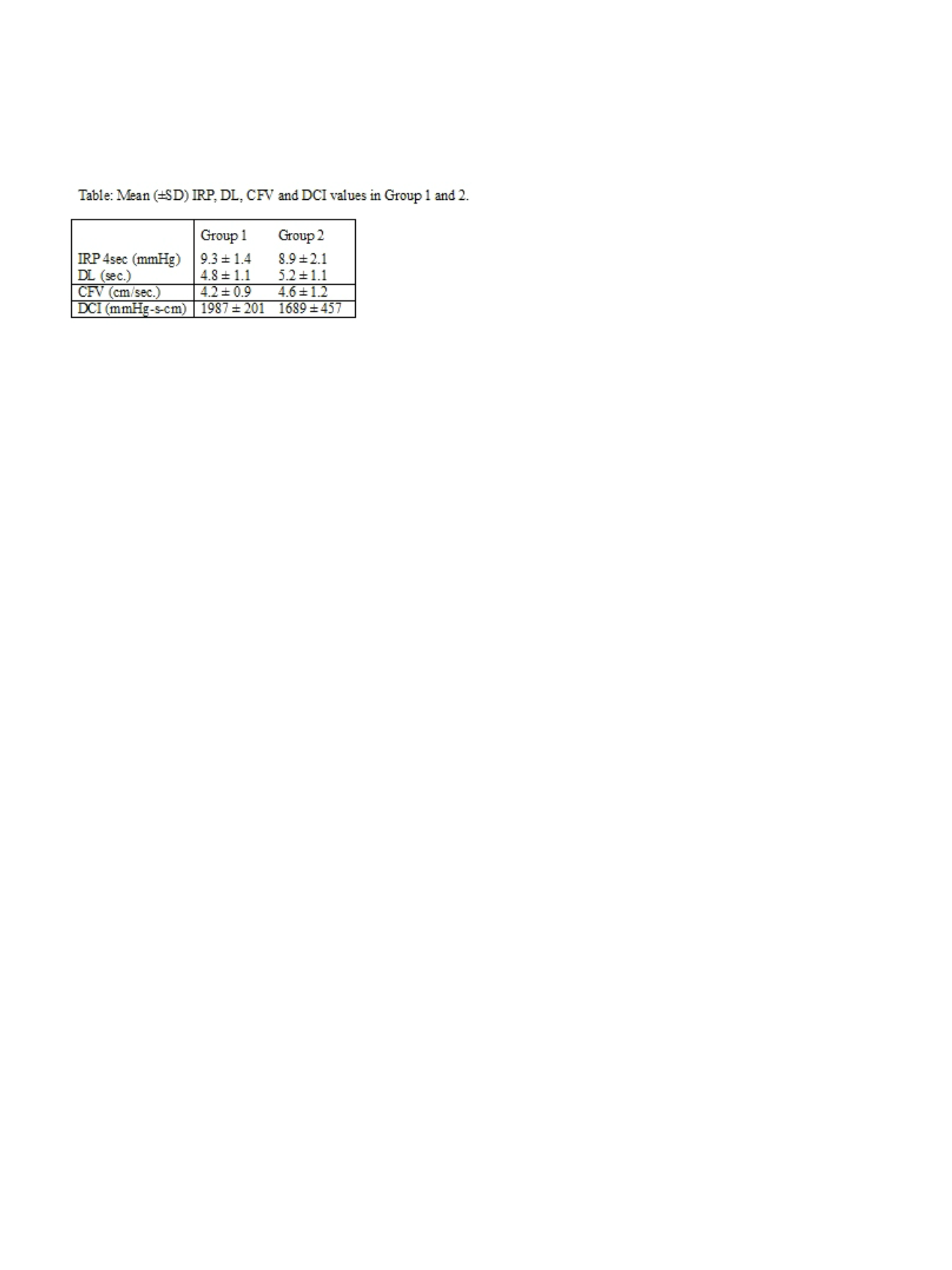
A total of 182 patients were enrolled (mean age 46.4 years,
mean follow-up 12.8 months, range 6-48 months). Fifty-two patients
(29%) had Type I achalasia, 112 (61%) Type II and 18 (10%) type III.
At univariate analysis significant differences were found among
patients with type I, type II and type III achalasia with regards
to basal LES pressure (33.3 mmHg, 47.9 mmHg and 57.3mmHg,
respectively. p<0.005), 4sIRP (26.7mmHg, 32.6mmHg and 33.2
mmHg, respectively. p<0.005) and esophageal diameter (5.2cm,
4.7cm and 3.6 cm, respectively. p<0.005).
No differences were found regarding age, gender, preoperative
symptoms, symptoms duration, previous treatments and esophageal
shape. At post-hoc analysis myotomy was significantly longer in
patients with type III achalasia (14.3±2.8cm) compared to type I
(10.9±2.3cm) or type II (11.4±2.2cm) (p<0.0001)
Success rate was similar in all patients, 96.2% for type I, 96.4% for
type II and 94.4% for type III achalasia (p ns).
Conclusions:
When myotomy is customized on HRM findings,
POEM outcomes do not significant differ in patients with type I, II
and III achalasia.
OC.05.7
LARYNGOPHARYNGEAL SYMPTOMS IN PRIMARY CARE:
USEFULNESS OF SALIVARY PEPSIN MEASUREMENT IN
PREDICTING GERD
Bozzani A.*
1
, De Bastiani R.
2
, Savarino E.
3
, Grattagliano I.
4
1
Gruppo Italiano di Gastroenterologia Ambulatoriale - Cure Primarie,
Monza, Italy,
2
Gruppo Italiano di Gastroenterologia Ambulatoriale -
Cure primarie, Feltre, Italy,
3
Division of Gastroenterology, Department
of Surgery, Oncology and Gastroenterology, University of Padua,
Padova, Italy,
4
Gruppo Italiano di Gastroenterologia Ambulatoriale,
Monopoli, Italy
Background and aim:
Incidence of chronic laryngeal symptoms in
primary care is 2%/year and, gastroesophageal reflux disease (GERD)
is considered by far the main factor associated to them, leading to
a specific syndrome called Laryngopharyngeal Reflux (LPR). Several
studies documented that pepsin measurement in saliva can be
adopted as surrogate marker of GERD in these patients. Recently, a
low cost, non-invasive salivary pepsin test (PeptestTM, RD Biomed
Limited, UK) has been shown to be able to measure pepsin in
the saliva/sputum and to discriminate with good sensitivity and
specificity between patients with typical GERD (i.e. with heartburn
and regurgitation) from those without and could be used to diagnose
LPR without pH monitoring, in primary care setting. We aimed to
investigate the usefulness of PeptestTM in primary care patients
presenting with chronic laryngeal symptoms suggestive of LPR.
Material and methods:
In a prospective multicenter, controlled,
pilot study, consecutive patients presenting with chronic laryngeal
symptoms were enrolled by primary care physicians. Uninvestigated
individuals with no gastrointestinal symptoms or disease (including
GERD) or history of surgery served as healthy controls (HCs). All
subjects completed RSI questionnaire and in case of a score >13 a
symptom-based diagnosis of LPR was made and GIS questionnaire
was completed to investigate reflux symptoms and Qol. All
individuals were asked to provide 2 samples of sputum collected one
hour after the two main meal. A positive PeptestTM was considered
in case of a concentration of pepsin higher than 25mg/mL.
Results:
Between February and April 2014 and during August 2015,
n=86 patients with LPR (37Male/49 Female, age 54±14; RSI≥13, mean
RSI 22±6, mean GSI 22±6.4) and 59 healthy controls (30M/29F, mean
age 41±15; RSI<5, mean RSI 0.5±1, mean GSI 33±5.6) were tested.
In total 256 samples were examined, whereas 34 samples were
discarded because of technical problems (i.e. unclear storage, poor/
excessive quantity). At least one positive result was found in 64/86
(74%) LPR patients and in 54/59 (92%) HCs (p<0.0095), whereas
two positive results were observed in 34/70 (49%) LPR patients and
26/46 (57%) HCs (p=0.4505). One (in case of a single test) or two
negative tests were registered in 22/86 (26%) LPR patients vs 4/59
(7%) of HCs (p<0.0039). PeptestTM had an accuracy of 47% (IC95
39%-55%) a sensitivity of 74% (IC95 65%-84%), a specificity of 7%
(IC95 0%-13%), a positive predictive value of 54% (IC95 45%-63%) and
a negative predictive value of 2% (IC95 0%-8%) in identifying LPR as
diagnosed by RSI.
Conclusions:
In this pilot study, PeptestTM was not able to
discriminate among primary care patients with LPR from those
without and therefore cannot be suggested as preliminary tool to
select patients requiring pH monitoring. Further studies including
investigated healthy controls are mandatory to elucidate the
diagnostic utility of salivary pepsin measurement in primary care
setting.


















