
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e87
PIG protocol (JPGN 2012;55:230-4); variables analysed: reflux
index, symptom index, number and type of liquid reflux, number
of long lasting reflux episodes, correlation symptom-reflux. The test
was diagnostic of GORD if at least ≥ 2 of the previous variables were
positive. The EHRM was performed with water perfused catheters
and swallow contractile patterns categorized using criteria recently
reported by a paediatric group (Am J Gastroenterol 2010;105:460-7).
Several motility variables were analysed: esophago-gastric junction
(EGJ) morphology, end-expiratory and end-inspiratory EGJ pressure,
distal contractile integral (DCI), pressurization front velocity (cm/s),
peristaltic propagation pattern.
Results:
An abnormal MII-pH profile was markedly more common
in GORD pts (27; 84.37%) than in EoE pts (4; 16%; p<0.001). On the
contrary, EHRM irregularities were detected more commonly in EoE
that the GORD pts: in particular, when motility tracing were
analysed no significant difference for EGJ pressure and deglutitive
EGJ relaxation was detected between the 2 groups; however,
abnormalities such as peristaltic dysfunction (i.e. failed peristalsis,
aperistalsis, and esophageal spasm features) and lower distal
contractile integral adjusted for esophageal body length (DCIa) were
more common in EoE (17; 68%) than in GORD pts (15; 46.8%)
(p<0.05).
Conclusions:
The great majority of EoE pts have a normal MII-pH
profile that doesn’t support the use of proton pump inhibitory
therapy. EoE pts exhibit higher prevalence of oesophageal motility
abnormalities than GORD: this feature is likely sustained by the
inflammatory infiltrate that characterizes the esophageal wall in
EoE and accounts for the esophageal dysmotility complaints often
detected in EoE pts.
OC.05.2
HIGH RESOLUTION MANOMETRY AND CLINICAL
CHARACTERISTICS OF PATIENTS WITH OUTFLOW OBSTRUCTION:
IS THIS A TRULY RELEVANT NOVEL MANOMETRIC DIAGNOSIS?
Russo S.*
1
, De Bortoli N.
1
, Tolone S.
2
, Martinucci I.
1
, Furnari M.
3
,
Frazzoni M.
4
, Bertani L.
1
, Surace L.
1
, Bellini M.
1
, Ricchiuti A.
1
,
Savarino V.
3
, Marchi S.
1
, Savarino E.V.
5
1
University of Pisa, Pisa, Italy,
2
Second University of Naples, Naples,
Italy,
3
University of Genoa, Genoa, Italy,
4
Baggiovara Hospital, Modena,
Italy,
5
University of Padua, Padua, Italy
Background and aim:
Recently the Chicago Classification (CC)
introduced a novel diagnosis to define the presence of impaired
relaxation of the lower esophageal sphincter and normal
peristalsis: the outflow obstruction (OO). However, limited high
resolution manometry (HRM) and clinical data are available on
the characteristics of patients presenting this manometric feature.
This study aimed to compare the characteristics of consecutive
patients with a manometric diagnosis of OO with those of a group of
patients with GERD. Secondary aim was to evaluate their reserve of
esophageal peristalsis by means of multiple rapid swallows (MRS).
Material and methods:
We included 21 patients with an HRM
diagnosis of OO, characterized by impaired EGJ relaxation (Integrated
Relaxation Pressure; IRP >15 mmHg) but preserved peristalsis
and 21 consecutive patients with GERD, as control group (CG). All
patients underwent HRM off-therapy. We evaluated esophagogastric
junction (EGJ) basal and maximal pressure, prevalence of
compartmentalized waves (pressurization of >30 mmHg extending
from the contractile front to the EGJ) and intra-bolus pressure (IBP)
in both groups. All patients underwent a provocative MRS (3 mL x 5
times consecutively). IRP and distal contractile integral (DCI) during
MRS were evaluated in both groups. The MRS/wet swallow ratio was
also calculated.
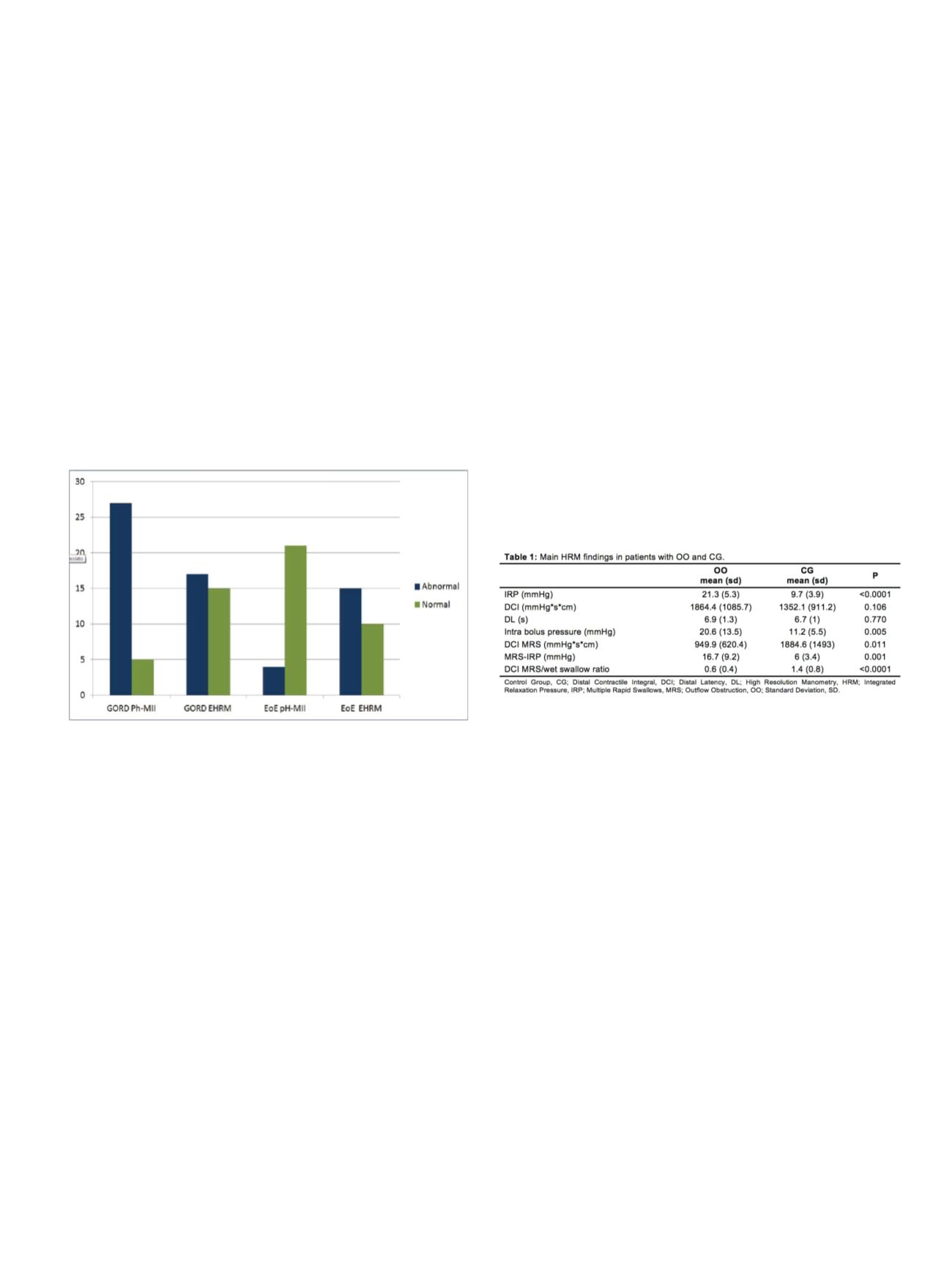
Results:
Mean age (58±14.4 vs 56.6±17.4), female (15 vs 12) and BMI
(24.2±3.2 vs 22.7±2.7) were similar in both groups (p=ns). Dysphagia
(100%) and regurgitation (59%) were prevalent symptoms in OO
group. Heartburn (100%) was the prevalent symptom in CG, whereas
dysphagia was absent and regurgitation (28.6%) was less frequent.
EGJ basal (32.6±11.6 vs 19.5±11.6) and maximal pressure (48.4±13.7
vs30.4±13.3)werehigherinOOgroup(p<0.001).Compartimentalized
waves were found in 71.4% of OO patients. As shown in Table 1, IBP
was higher in OO group (p<0.005). DCI-MRS was two times higher in
CG than in OO group. IRP during MRS decreased under 15 mmHg in
9/22 (40.9%) of patients with OO. DCI MRS/wet swallow ratio was >1
in 20/21 patients from CG but only in 3/21 in OO group.
Conclusions:
In our cohort, the diagnosis of OO was associated with
the presence of obstructive symptoms (dysphagia±regurgitation)
as major complain supporting the relevance of this manometric
diagnosis which can be achieved by HRM. Moreover, the reserve
of esophageal function evaluated with MRS and MRS/wet swallow
ratio showed a reduction in OO group.
OC.05.3
NERD AND PH CYCLICAL FLUCTUATION: PROPOSED OF THE IDEAL
DIAGNOSTIC ALGORITHM
Scarpulla G., Scalisi G.*, La Ferrera G., Garufi S., Manganaro M.,
Camilleri S.
Ospedale M. Raimondo, San Cataldo, Italy
Background and aim:
Non-Erosive Reflux Disease (NERD) is the
most common phenotypic manifestation of Gastroesophageal Reflux
Disease (GERD) and includes patients who have typical symptoms
without mucosal alterations at endoscopy. These patients are
pathophysiological extremely heterogeneous and must be properly
classified.
Aim of our study is to demonstrate the cyclical fluctuation of pH
in patients with NERD and therefore the need to investigate them
through prolonged ambulatory pH monitoring and only negative
patients by pH impedance.
Material and methods:
From September 2013 to September 2015
300 patients with NERD (excluded esophageal injury by endoscopy)
were included in our prospective study. Prolonged ambulatory pH
monitoring (72/96 h) by Bravo system were performed in all of 300


















