
e82
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
OC.03.6
ANTICOAGULATION THERAPY FOR NON MALIGNANT
PORTAL VEIN THROMBOSIS IN CIRRHOTIC PATIENTS: A SAFE
TREATMENT?
Sbrancia M.
1
, Antonelli E.
2
, Bassotti G.
1
, Clerici C.
2
, Morelli O.*
1
1
Gastroenterology Section, Medicine Department, University of
Perugia, Perugia, Italy,
2
Gastroenterology Section, Perugia General
Hospital, Perugia, Italy
Background and aim:
Non-neoplastic portal vein thrombosis
(PVT) is a frequent event in cirrhotic patients but its natural
history is poorly understood. It can be treated with anticoagulants,
however the safety and efficacy of this therapeutic approach are
still unknown. We performed a retrospective study evaluating the
effect of anticoagulants in a series of cirrhotic patients with non-
neoplastic PVT.
Material and methods:
A retrospective ultrasound chart review
of cirrhotic patients seen in our Liver Unit between February 2008
and March 2015 was performed. Subjects with non-neoplastic PVT
(defined as the absence of invasion or infiltration of the portal vein by
neoplasia) were identified by reviewing US and TC reports. Partial vs
complete PVT was considered as the absence or presence of power-
Doppler signal at the ultrasound. Demographic, clinical, laboratory,
endoscopic parameters and thrombophilia screening were analyzed.
Dose, duration, efficacy and side effects of anticoagulant therapy
were also evaluated.
Results:
Charts of 375 cirrhotic patients of any etiology were
evaluated. Non-neoplastic PVT was identified in 28 cases (7,5%) and
it was mostly partial. Low platelet count, high MELD score (13±4),
Child-Pugh class B or C and esophageal varices were the most
frequent characteristics of these patients. Trombophilic disorders
(antithrombin deficiency, protein C deficiency, protein S deficiency,
presence of Lupus Anticoagulant antibodies) were observed in 9
patients; 16 patients received anticoagulation therapy (low-weight
heparin or warfarin) for 3-6 months and 12 patients received no
treatment. Partial or complete recanalization was achieved in 12
anticoagulated patients (75%), while in 3 patients (25%) spontaneous
improvement of PVT (p=0,025) was observed. The recurrence of
thrombosis was seen in 43% patients after stopping anticoagulation
therapy. Five anticoagulated patients developed bleeding complica
tions but no deaths were observed. Ten patients without treatment
developed liver-related events (portal hypertension-related
bleeding, ascites, hepatic encephalopathy) and 4 patients died.
Conclusions:
In our study, anticoagulation therapy is a safe
treatment for PVT, leading to recanalization of the portal vein in 75%
of patients. It seems to be reasonable to maintain indefinitely the
anticoagulation therapy to prevent thrombosis recurrence.
OC.03.7
CIRCULATING MICROPARTICLES AND RISK OF PORTAL VEIN
THROMBOSIS IN PATIENTS WITH LIVER CIRRHOSIS AND
HEPATOCELLULAR CARCINOMA
Zanetto A.*
1
, Ferrarese A.
1
, Nadal E.
1
, Bortoluzzi I.
1
, Russo F.P.
1
,
Germani G.
1
, Campello E.
2
, Spiezia L.
2
, Simioni P.
2
, Burra P.
1
,
Senzolo M.
1
1
Multivisceral Transplant Unit, Padua, Italy,
2
V Chair of Internal
Medicine, Padua, Italy
Background and aim:
tudies which explore the hypercoagulable
state associated with this hepatocellular carcinoma (HCC) and its
correlation with the risk of portal vein thrombosis (PVT) are lacking.
We investigated the presence and cellular origins of circulating
microparticles (MP) of different cellular origins in plasma from
patients with cirrhosis with and without HCC evaluated the possible
contribution of MP to PVT occurrence in HCC patients.
Material and methods:
Plasma levels of annexin V MP, endothelial-,
platelet- and leukocyte-derived MP, tissue factor-bearing MP and
thrombomodulin-bearing MP were measured by cytoflowrimetry
in 65 adult cirrhotic patients, 33 with and 32 without HCC. PVT
occurred in 12 (18%) cirrhotic patients, 8 with HCC and 4 without
HCC. Fifty healthy subjects used as controls.
Results:
Patients with cirrhosis and HCC had significantly higher
median plasma levels of MP than patients with cirrhosis without
HCC and healthy controls. Patients with HCC and cirrhosis who
developed PVT showed significantly higher median plasma levels
of annexin V MP and endothelial-derived MP than patients with
cirrhosis and HCC who did not developed PVT. MP were associated
with a higher but not statistically significant RR for PVT. Cirrhotic
patients without HCC showed significantly higher median levels of
MP compared to healthy controls.
Conclusions:
Hypercoagulability as assessed by circulating plasma
MP levels is clearly present in cirrhotic with HCC patients and may
contribute to the PVT occurrence. The “degree” of hypercoagulabity
increases from cirrhosis alone to cirrhosis with HCC.
OC.03.8
DRUG-ELUTING BEADS VERSUS CONVENTIONAL
CHEMOEMBOLIZATION FOR THE TREATMENT OF
HEPATOCELLULAR CARCINOMA: A META-ANALYSIS
Facciorusso A.*, Di Maso M., Muscatiello N.
University of Foggia, Foggia, Italy
Background and aim:
Despite the promising results of earlier
studies, a clear superiority of drug-eluting beads transarterial
chemoembolization over conventional chemoembolization has
not been established yet. Aim of this meta-analysis is to evaluate
the efficacy and safety of the two treatments in hepatocellular
carcinoma patients.
Material and methods:
Computerized bibliographic search on the
main databases was performed. One-year, two-year, three-year
survival rates were analyzed. Hazard ratios from Kaplan-Meier
curves were extracted in order to perform an unbiased comparison
of survival estimates. Objective response and severe adverse event
rate were analyzed too. Comparisons between the two treatments
were performed by using Mantel-Haenszel test in case of low
heterogeneity or DerSimonian and Laird test in case of high
heterogeneity. The results were expressed as odds ratio and 95%
confidence interval.
Results:
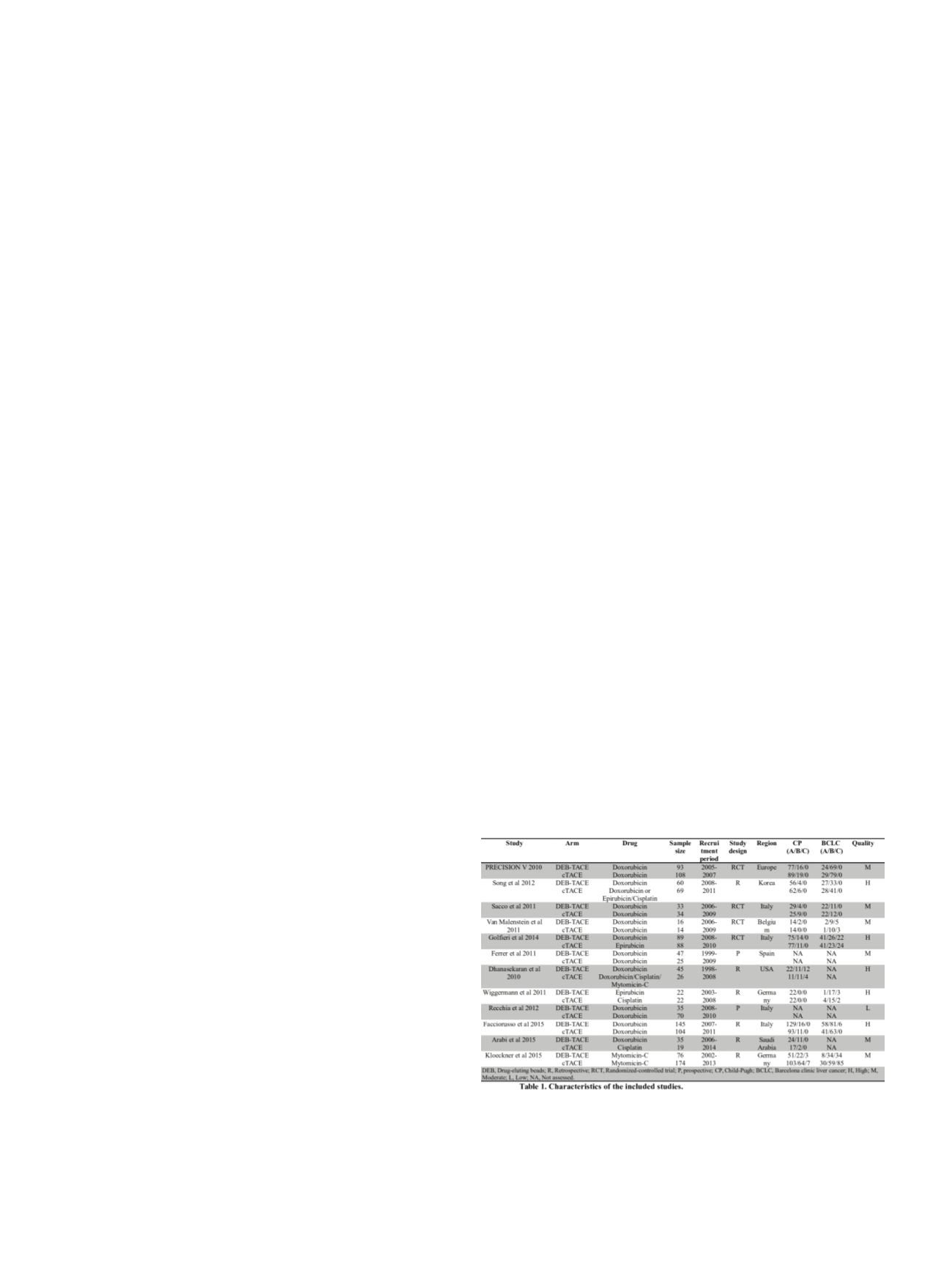
Four randomized-controlled trials and 8 observational
studies with 1449 patients were included in the meta-analysis
(Table 1). Non-significant trends in favor of drug-eluting beads
chemoembolization were observed as for 1-year (odds ratio: 0.76,
0.48-1.21, p=0.25), 2-year (odds ratio: 0.68, 0.42-1.12, p=0.13) and


















