
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e85
after polypectomy, but the interaction between these factors is
still unclear. We aimed to generate a prognostic model for post-
polypectomy ACA recurrence by defining different prognostic
groups.
Material and methods:
Out of 3360 patients who underwent colon
polypectomy at University of Foggia between 2004 and 2008, data of
843 patients with 1155 ACAs was retrospectively reviewed. Recursive
partitioning analysis of predictors for 3-year post-polypectomy
recurrence was performed.
Results:
Median ACA size was 16 mm (interquartile range 12-23)
while their median number was 1.5 (1-2). Pedunculated, sessile and
non-polypoid lesions were 40.9%, 39.6% and 19.5% of ACAs detected,
respectively. Independent predictors of 3-year recurrence were
lesion size [odds ratio (OR): 3.96, 95% confidence interval: 1.87-7.55,
p<0.001], number (OR: 3.22, 2.19-5.39; p<0.001) and grade of
dysplasia (OR: 4.25, 2.11-7.50); p<0.001), as confirmed both in
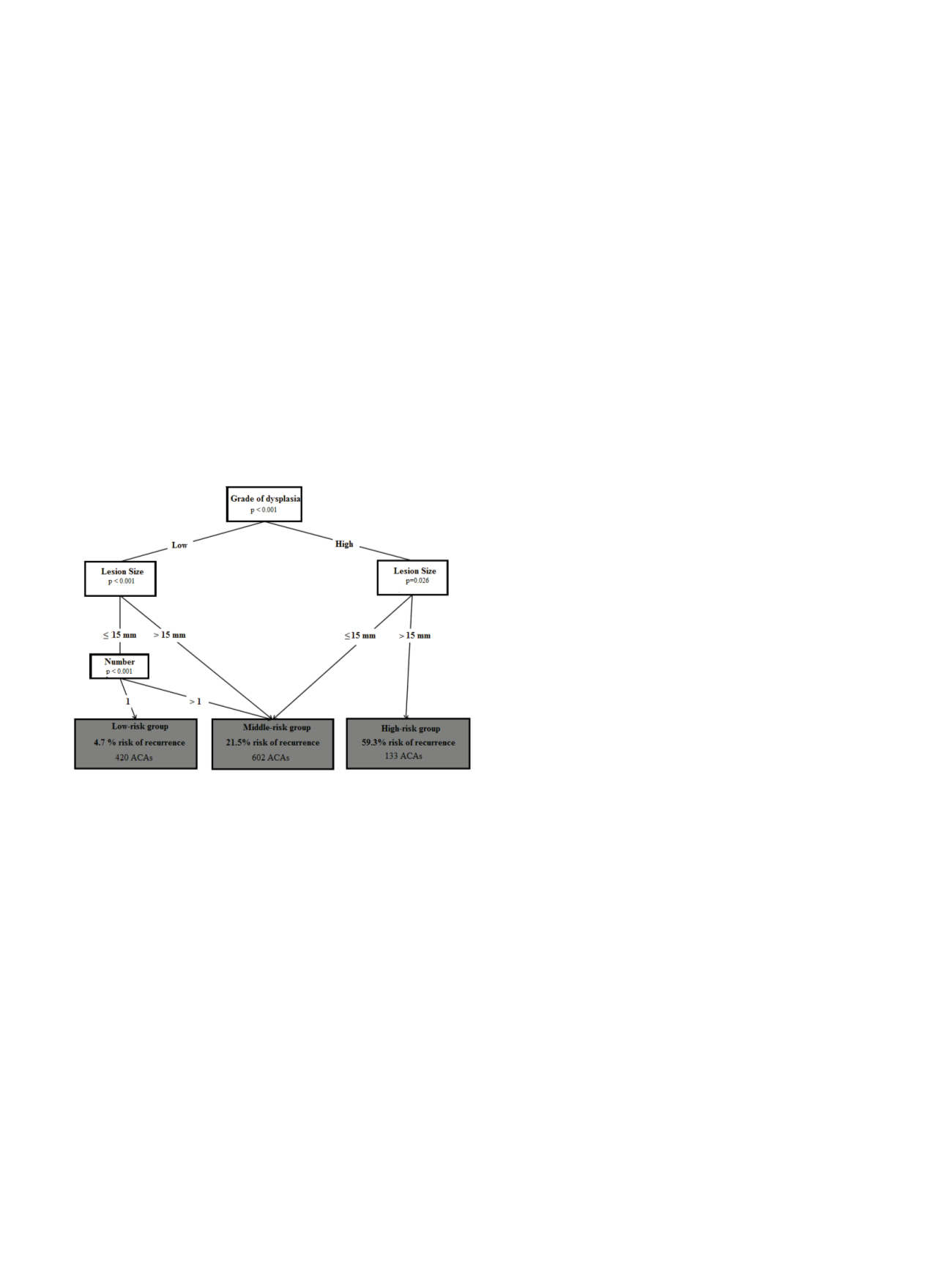
logistic regression and in random forest analysis. Recursive
partitioning analysis identified three risk groups: low-risk in
presence of single ACA ≤15 mm with low-grade dysplasia (LGD),
medium-risk in case of high-grade dysplasia (HGD) ≤15 mm, LGD
>15 mm or multiple LGDs ≤15 mm, and high-risk if HGD >15 mm
(Figure 1). Three-year recurrence rate was 4.7%, 21.5% and 59.3%,
respectively (p<0.001).
Conclusions:
ACAs ≥15 mm presenting HGD are at higher risk of
recurrence and might benefit from more intensive surveillance,
while single LGD ≤15 mm could be considered for longer follow-up
intervals.
OC.04.6
EARLY DETECTION OF METACHRONOUS COLORECTAL CANCER:
THE ROLE OF FATTY ACID SYNTHASE (FASN)
Riga C.
1
, Corazziari E.*
1
, Murari R.
2
, Pedullà G.
1
, Pronio A.
1
, Covotta A.
1
,
Lamazza A.
1
, De Toma G.
1
, Alò P.L.
2
, Rivera M.
1
1
Policinico Umberto I, Roma, Italy,
2
ospedale Umberto I, Frosinone,
Italy
Background and aim:
Patients undergoing curative resection
of colorectal cancer have an increasing risk (from 0.6 up 9%) to
develop a metachronous tumor, being this risk higher in the first
3 years following the diagnosis. Therefore, it would be desirable
that non invasive investigations such as those based on the
analysis of markers can detect, after a therapeutic resection of
a CRC, the patients who have an increased risk of developing
a second tumor, in order to restrict the most frequent controls
only to these cases. In this study, the following markers will be
evaluated with immunohistochemistry: ki-67, a nuclear protein
which is used as an index of cell proliferation; bcl-2 an oncoprotein,
whose overexpression plays a role in the early stages of colorectal
carcinogenesis; p-53,“the guardian of the genome”, and FASN, an
enzyme that catalyzes the synthesis of long-chain fatty acids, which
are considered as a late marker of tumor progression.
The aim is to evaluate whether the expression of biological markers
such as p53, bcl-2, Ki-67 and FASN on healthy colon mucosa is
predictive of onset, presence or absence of metachronous cancer.
Material and methods:
In a prospective study consecutive
outpatients or inpatients diagnosed with CRC stage I-III were
recruited. Patients with HNPCC or IBD were excluded. All patients
underwent periodic colonoscopies during which biopsies were
performed on healthy mucosa in pre-defined colic sections. The
biological markers were assessed with immunohistochemistry on
biopsy samples.
Results:
In three year observation time a total of 16 patients
(age: 53-83 years old, M:F 8:8) were examined. Three patients
were diagnosed with synchronous lesions, four patients with
metachronous lesions and one patient experienced recurrence of
the disease. A patient, whose FASN was already positive on a healthy
colon mucosa, developed a metachronous lesion on the same site
of the positive biopsy, while in case of patients with synchronous
lesions or recurrent disease, the FASN became positive at the
same time such lesions were detected. None of the others markers
investigated were detected during the study period.
Conclusions:
The expression of FASN on healthy colon mucosa
suggests that colon cells can transiently modify their metabolism
in order to gain a greater input of energy. Therefore, the finding of
its positivity, as reported in this study, may indicated an increased
risk to develop a metachronous lesion and the need to submit such
patients to a more intensive follow-up.
OC.04.7
IDENTIFICATION OF PROTEOMIC PROFILES ASSOCIATED WITH
TUMOR REGRESSION GRADING IN RECTAL CANCER
De Re V.*, Repetto O., De Paoli A., Fornasarig M., Maiero S.,
Buonadonna A., Belluco C., Orzes E., Zucchi E., Canzonieri V.,
Cannizzaro R.
Centro di Riferimento Oncologico, Aviano, Italy
Background and aim:
Rectal cancer response to neoadjuvant chemo-
radiotherapy (CRT) is variable. Identifying markers of response will
help select patients more likely to benefit from therapy. Objective
of the study is to identify at diagnosis proteomic profiles associated
with tumor regression grading (TRG) in rectal cancer.
Material and methods:
This study includes 40 patients with rectal
cancer treated with CRT followed by surgery. Proteins from pre-
treatment tumor biopsies and control from paired normal bioptical
specimens were screened for comparative proteomic approach by
using 2D difference gel electrophoresis (2D-DIGE). Differential spots
found with Decyder were identified by MALDI-TOF and peptide
fingerprinting with Mascot search engine. Interactions among
identified proteins were analyzed with STRING 9.1 search tool.
Pathological TRG was assessed on surgical specimens.
Results:
A total of 30 proteins were identified as discriminators
between tumor samples and controls by principal component
analysis and hierarchical clustering (p<0.01; spot map>50%). These
proteins were already described as involved in rectal metabolic cell
pathways and angiogenesis. Possible correlations between these
proteins and TRG are under evaluation.
Conclusions:
Comparative proteomics approach based on 2D-DIGE
and MALDI-TOF identification succeeded in differentiating rectal
tumor samples from paired normal rectal mucosa. Further analyses
will unravel possible correlations between distinct protein profiles


















