
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e133
P.01.8
PERCUTANEOUS ELECTROCHEMOTHERAPY OF MALIGNANT MAIN
PORTAL VEINS THROMBOSIS: A PROSPECTIVE CASE SERIES
Tarantino L.*
2
, Busto G.
1
, Nasto A.
3
, Fristachi R.
4
, Talamo M.
5
,
Ambrosino P.
6
, Tarantino P.
6
, Accardo C.
5
1
Medical Oncology Unit - “A.Tortora” Oncology Hospital, Pagani
(SA), Italy,
2
Interventional Hepatology Unit - “A.Tortora” Oncology
Hospital, Pagani (SA), Italy,
3
General and Oncologic Surgery Unit -
“A.Tortora” Oncology Hospital, Pagani (SA), Italy,
4
Anatomic Pathology
Department - “A.Tortora” Oncology Hospital, Pagani (SA), Italy,
5
Radiology Department - “A.Tortora” Oncology Hospital, Pagani
(SA), Italy,
6
Department of Clinical Medicine and Surgery, Federico II
University, Naples, Italy
Background and aim:
Cirrhotic patients with malignant main portal
vein thrombosis (MMPVT) from hepatocellular carcinoma (HCC) are
excluded fromanyknowncurative treatment. Asingleprevious report
advocated a possible role of Radiofrequency Thermal Ablation (RF).
Electrochemotherapy (ECT) is a non-thermal local tumor ablation
modality using electroporation, a physical method that enhances
cell membrane permeability, and enables chemotherapeutic agents
to enter tumor cells. This technique is virtually able to damage
tumor cells without affecting stromal structures and normal cells
proximal to the tumor. In order to evaluate the effectiveness and
safety of the technique, we treated with ECT, in a prospective study,
a series of patients with liver cirrhosis and MMPVT from HCC.
Material and methods:
Six patients were enrolled. All of them
underwent pre-treatment three-phase abdominal computed
tomography (CT), contrast enhanced ultrasound (CEUS), and
ultrasound (US) guided percutaneous biopsy of the thrombus. We
performed ECT in general anesthesia, with intubation. Under US
guidance, four to six electrode-needles were inserted percutaneously
along the external margin of the thrombosed portal vessel. The
electrodes were connected to independently controlled generator
outputs of the Cliniporator Vitae (IGEA, Carpi, Italy). 8 minutes after
intravenous injection of a Bleomicin bolus (15,000 IU/m2), electric
pulses were delivered. All patients underwent percutaneous US
guided biopsy of the treated tumor. Short term control of efficacy of
the ECT was performed with intraoperatively CEUS, at the end of the
procedure, and an additional CEUS after 24 hours. All patients were
followed up with monthly color-doppler US (CDUS) and CEUS for
six months. Three-phase CT was repeated as soon as CDUS showed
recanalization of treated portal vein.
Results:
The follow-up ranged from 2 to 9 months. Monthly post-
treatment CEUS demonstrated complete absence of enhancement
of the thrombosis in all cases. Pre-treatment biopsy was adequate
and showed viable HCC in 4/5 cases. Post treatment biopsy showed
severe involutive changes of tumor cells with cellular apoptosis
and areas of necrosis. In 2 cases, the specimen included the portal
vein wall that showed normal endothelium and normal stromal
aspects of the wall. The first patient (9 months follow-up) showed a
completely patent portal vein at CDUS, CT and CEUS within 2 months
from the ECT. 2 patients (6 and 5 months follow-up) showed partial
recanalization of the treated portal vessel. The other 3 patients (2, 5,
and 3 months follow-up, respectively) showed avascular thrombus
at monthly CEUS and CDUS, and at 2-month CT.
Conclusions:
ECT seems an effective and safe procedure for curative
treatment of MMPVT. This technique does not affect hilar biliary
structures and vessels. Results on larger series of patients are needed
to confirm these preliminary results.
P.01.9
THE GUT MICROBIOTA OF CIRRHOTIC PATIENTS WITH POOR
NUTRITIONAL STATUS: PRELIMINARY EVIDENCES
Ponzani F.R.*
1
, Pecere S.
1
, Petito V.
1
, Paroni Sterbini F.
2
, Tortora A.
1
,
Annichiarico B.E.
1
, Siciliano M.
1
, Palladini A.
2
, Graziani C.
1
,
Masucci L.
2
, Pompili M.
1
, Sanguinetti M.
2
, Gasbarrini A.
1
1
Internal Medicine and Gastroenterology, A Gemelli Hospital, Rome,
Italy,
2
Microbiology, A Gemelli Hospital, Rome, Italy
Background and aim:
Gut microbiota (GM) modifications have
been reported in malnourished populations. Liver cirrhosis is often
associated with malnutrition and sarcopenia but GM changes in this
setting have not been investigated yet.
The aim of the present study was to investigate changes in GM
composition according to nutritional status in patients affected by
liver cirrhosis.
Material and methods:
Fecal samples of cirrhotic patients without
exposure to antibiotics, pre-/pro-biotics and bowel colonoscopy
preparation for at least one month were collected. Nutritional status
was assessed by a multi-dimensional questionnaire including
clinical and anthropometric parameters (Mini Nutritional
Assessment, MNA). GM composition was assessed by a metagenomic
gene-targeted approach (16S rRNA) using the Roche 454 GS Junior
and Qiime pipeline. Biostatistic analysis was performed using
R-statistics packages.
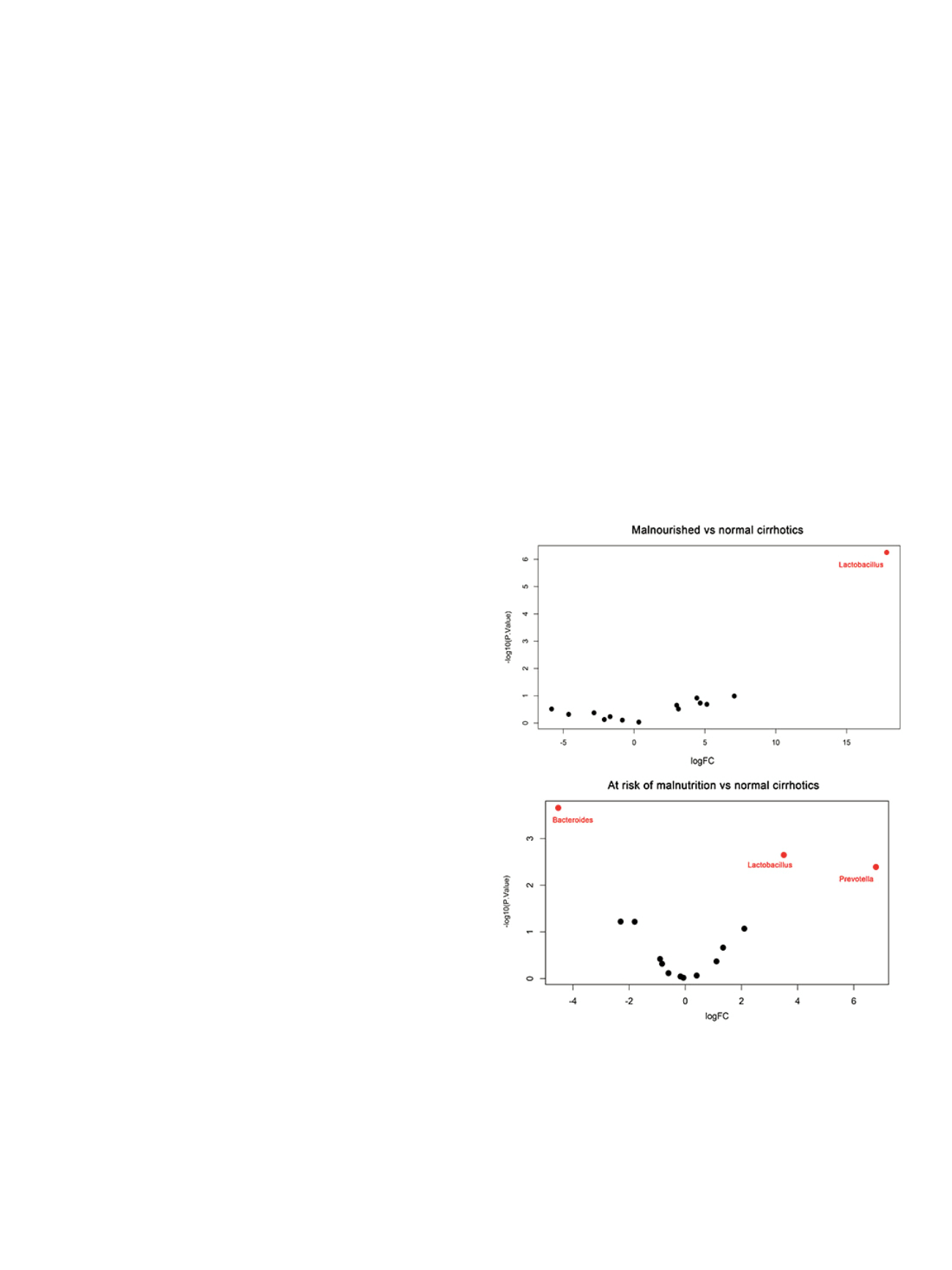
Results:
Twenty cirrhotic patients were included in the study;
median age was 60 years, Child-Pugh A/B/C 10/4/6, 13 (65%) were
well-nourished, 5 (25%) at risk of malnutrition and 2 (10%) severely
malnourished according to MNA. Nonmetric multidimensional
scaling (NMDS) ordination on Bray Curtis distance revealed a
significant clustering according to nutritional status rather than to
Child-Pugh score (p=0.014 vs p=0.06 PERMANOVA). Malnutritionwas
associated with increased abundance of Lactobacillus and Prevotella
and a reduction in Bacteroides (adj. p-value <0.05; Figure 1). This


















