
e132
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
Background and aim:
Hepatic encephalopathy (HE) is considered
reversible regarding mental status (alertness, orientation) but may
not be from a cognitive standpoint (performance on specialized
tests that reflect daily function). Poor cognitive function despite
treatment for HE has been shown in single-center studies. The aim
of this study was to evaluate persistence of cognitive impairment in
patients treated for HE compared to those who never experienced
HE (no-HE) patients in a multi-center study.
Material and methods:
174 outpatient cirrhotics from 3 centers
(94 subjects from Virginia, 30 from Ohio and 50 from Rome, Italy)
underwentcognitivetestusingPsychometrichepaticencephalopathy
score (PHES) and Inhibitory control test (ICT); patients were tested
at baseline and re-tested at least 7 days apart without intervening
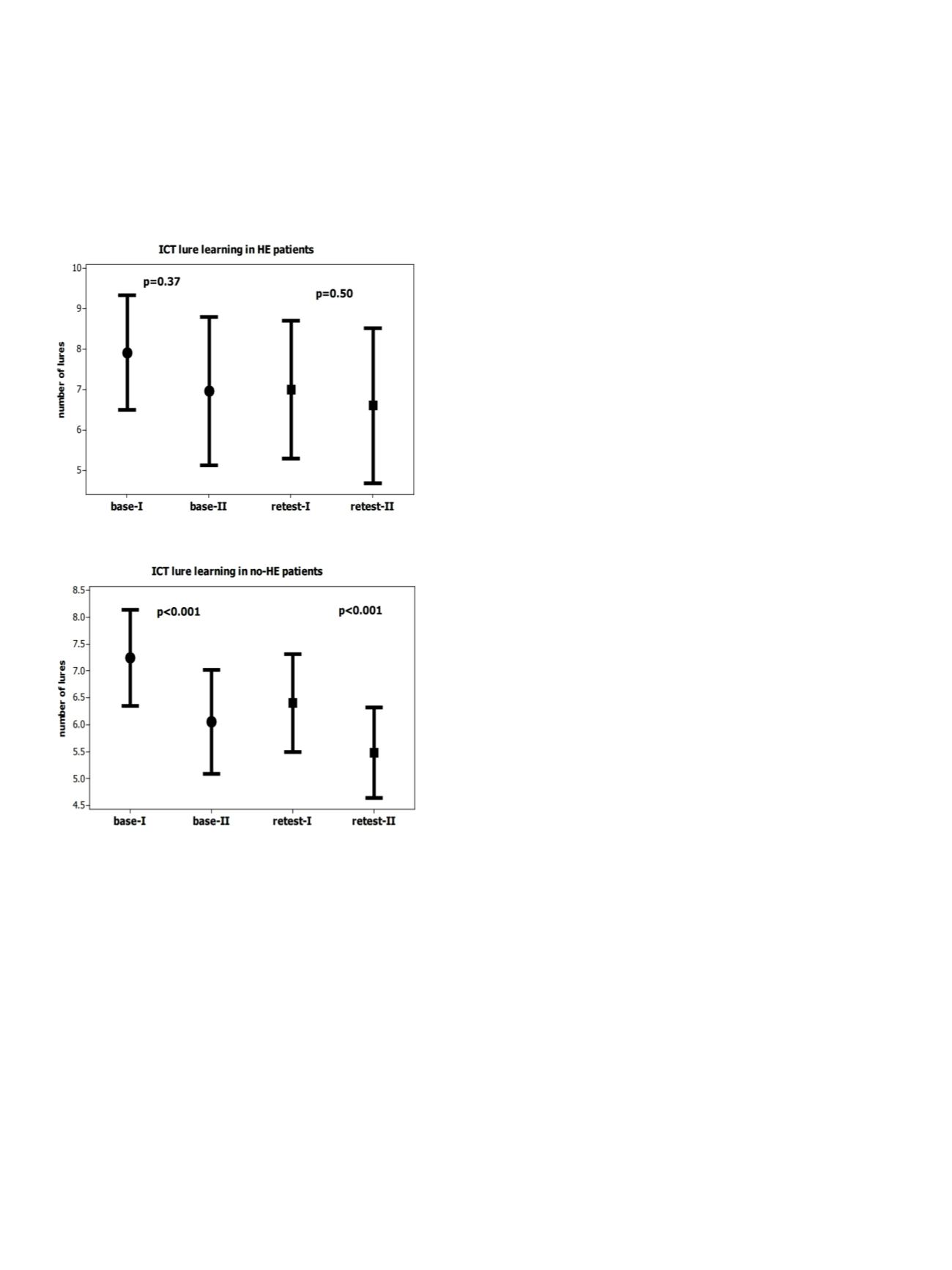
change in liver disease severity. ICT learning (change in 2nd half
lures compared to 1st half) was compared between HE and no-HE
patients at baseline and at the re-testing visits.
The changes in the PHES individual sub-tests between baseline and
re-testing visits were compared between HE and no-HE patients.
Results:
Thirty six patients had prior HE; all were controlled on
lactulose and 9 were on additional rifaximin. All HE patients were
completely alert and oriented at the time of the testing (mini-
mental score >25). HE patients had a higher MELD score compared
to no-HE patients (16 vs. 10, p<0.0001). HE patients had worse
performance on all tests compared to no-HE patients at baseline;
a significant improvement (learning) (1st half 7.1 vs. 6.2, 2nd half,
p<0.0001) was observed in no-HE patients and not in HE patients
(1st half 7.9 vs. 7.8, p=0.1). All patients were retested a median of
20 days later without change in cirrhosis severity, medications or
complications. No HE patients had significant learning or reduction
in lures (1st half 6.0 vs. 2nd half 5.4, p<0.0001), while in HE patients
again did not show ICT learning (1st half 7.8 vs. 2nd half 6.9, p=0.37).
As regards Psychometric Hepatic Encephalopathy Score (PHES), no-
HE patients shown an improvement in 4 PHES sub-tests instead of
HE patients had an improvement only in 2 PHES sub-tests.
Conclusions:
In this multi-center study, patients with prior HE
showed persistent significant learning impairment compared to
those without prior HE, despite adequate medical therapy. This
persistent change should increase efforts to reduce the first HE
episode.
P.01.7
MICROWAVE ABLATION OF LARGE HCCS BY SIMULTANEOUS
MULTIPLE ANTENNAE INSERTION: LONG TERM FOLLOW-UP
Tarantino L.*
1
, Ambrosino P.
2
1
Interventional Hepatology Unit - “A.Tortora” Oncology Hospital,
Pagani (SA), Italy,
2
Department of Clinical Medicine and Surgery,
Federico II University, Napoli, Italy
Background and aim:
To report long term results of microwawe
(MW) ablation with simultaneous insertion of multiple antennae
for large hepatocellular carcinoma (HCC).
Material and methods:
Between October 2008 and September
2013, 36 cirrhotics with a single HCC nodule >3 cm (range :3.2-
7.0cm; mean: 4.4 cm) underwent MW ablation in a single session
by simultaneous insertion of multiple 13-gauge-MW-antennae
(Viva-Wave, Covidien, USA). All patients underwent intraoperative
evaluation of efficacy with contrast enhanced ultrasound (CEUS).
Residual viable tumor at CEUS was treated in the same session by
reinsertion of 2-3 MW antennae in the tumor. Efficacy of ablation
was definitely assessed with three-phase computed tomography
(CT) after one month. After treatment, scheduled follow-up entailed
US every 3 months and CT every 12 months.
Results:
10 and 18 patients were treated with a single insertion
of 2 and 3 synchronous antennae, respectively. 8 patients were
treated with 2 insertions of 3 antennae in the same session.
Intraoperative CEUS showed residual tumor in 12 patients. 9
out of these patients underwent an additional insertion of two
antennae and 3 patients of three antennae. Intraoperative CEUS at
the end of the procedure showed complete necrosis in all patients.
1month-CT showed complete necrosis in 33/36 patients. A severe
hemoperitoneum, treated with blood transfusion, occurred in one
patient after treatment. No major complication occurred in the
other patients. Follow-up ranged from 18 to 78 months (mean: 42
months). During follow-up, local recurrence occurred in 7 patients
within 3 to 12 months (mean: 6 months). Recurrences in other liver
segments occurred in 35/36 patients within 6 to 24 months (mean:
15 months). Extrahepatic metastasis from HCC were observed in
1 patient 24 months after treatment. 16 patients died within 18-
60 months (mean: 36 months), for tumor progression in 11 cases,
decompensation of cirrhosis in 4 cases, hemorrhagic stroke in 1
case, respectively. 20 patients were alive at 18-78 months follow-up
(mean: 42 months).
Conclusions:
Ablation of large HCC by simultaneous insertion of
multiple MW antennae is a safe and effective treatment and can
result in long survival of patients.


















