
e138
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
The aim of this study was the evaluation of pancreatic exocrine
insufficiency (PEI) in patients with stable IPMN (Main Duct, Branch
Duct and combined) with evidence of a widespread involvement of
the pancreatic gland.
Material and methods:
Eighty-nine patients with magnetic reso
nance cholangiopancreatography (MRCP) findings of cystic lesions
compatible with IPMN were evaluated. Patients with other possible
causes of PEI (pancreatic or gastric resection, diabetes mellitus,
inflammatory bowel disease and celiac disease, etc.) were excluded.
Twenty six patients with 3 or more cystic lesions were enrolled and
followed up for at least 1 year. Exocrine pancreatic function was
evaluated by determination of fecal elastase-1 (FE‑1). A five degree
radiological score system, based on MRCP, was specifically created
to judge glandular involvement (Table 1).
Table 1
Degree of glandular involvement of IPMN
Degree 1
Millimeter ductal ectasia
Degree 2
Few moderately diffuse ductal ectasia
Degree 3
Diffuse ductal ectasia
Degree 4
Ductal ecstasia with glandular hypotrophy
Degree 5
Main duct ectasia and/or severe glandular subverting
Results:
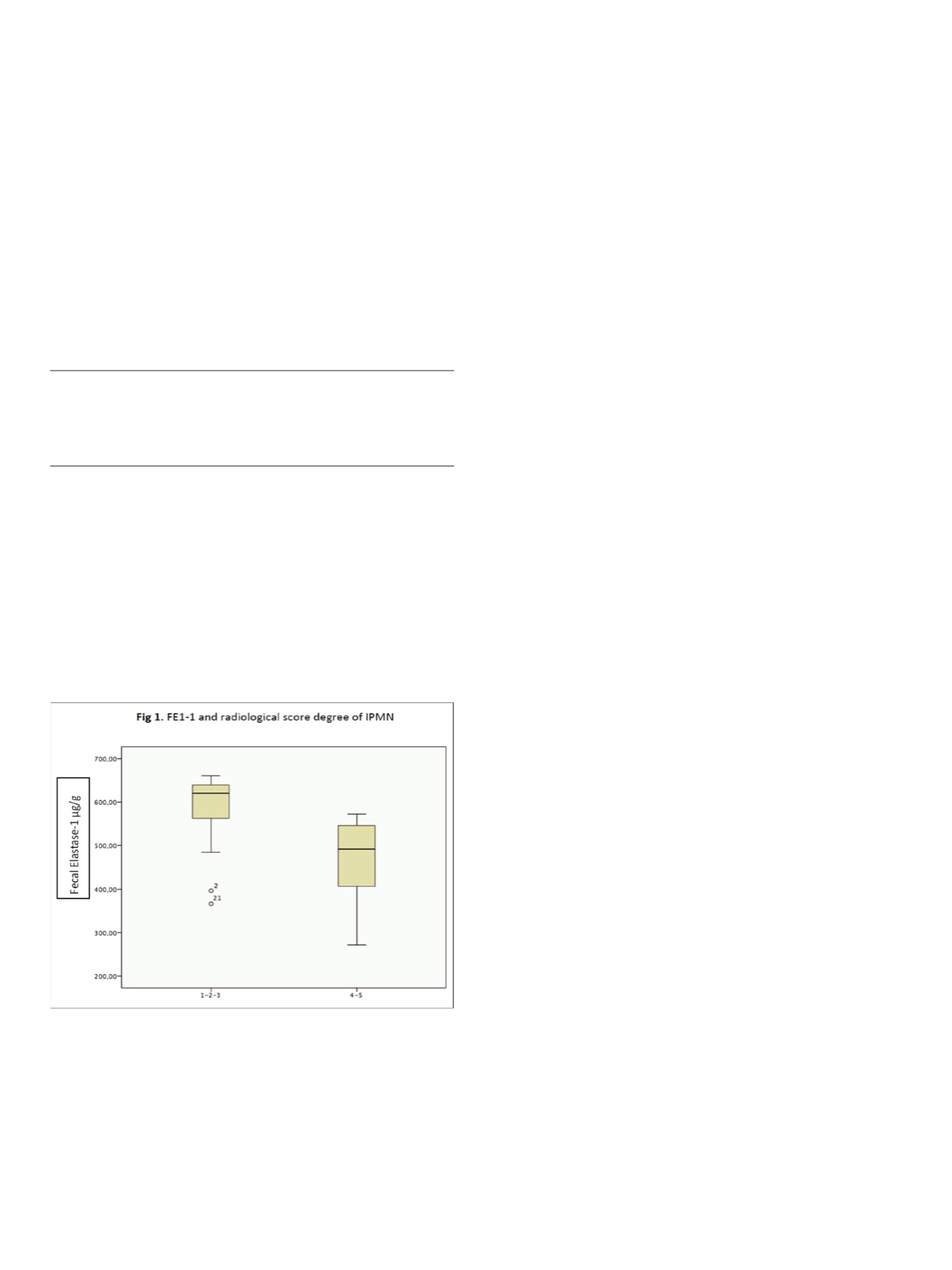
The Pearson test was used to correlate FE-1 values with age.
The Spearman test was used to correlate FE-1 with the radiological
score. The ANOVA test was used to evaluate mean FE-1 values for
each involvement degree. Statistical significance was set at p<0.05.
Mean FE-1 values were 539.4±111.5 µg/g. FE-1 was inversely related
to age (r=-0.465; p=0.017) and to radiological score system (rs=-
0.478; p=0.013). Mean FE-1 values, adjusted for age, were
significantly lower in patients with more severe glandular
involvement, such as pancreatic atrophy and main duct or combined
type (degree 4-5), than in patients with a mild to moderate degree
(different degrees of impairment by BD-IPMN; degree 1,2 and 3)
(p=0.003) (Fig. 1).
Conclusions:
Patients with more severe glandular involvement,
such as pancreatic atrophy and main duct ectasia, have lower values
of FE-1. Further studies on a larger number of patients with a high
degree of IPMN glandular involvement could identify different
conditions of IPE.
P.02.12
THE USE OF COMPLEMENTARY AND ALTERNATIVE MEDICINE IS
FREQUENT IN PATIENTS WITH PANCREATIC DISORDERS
Stigliano S.*, Archibugi L., Zerboni G., Delle Fave G., Capurso G.
Ospedale Sant’Andrea, La Sapienza, Roma, Italy
Background and aim:
Herbal remedies and other not conventional
medicines (CAM) arewidely used for the treatment of various chronic
diseases including gastrointestinal and liver disorders. Some 30% of
patients with liver disease and inflammatory bowel diseases have
been reported to use CAM. CAM users are mainly women, with high
education level. The most common reason for use is dissatisfaction
with conventional care. However, there are no data regarding CAM
use in patients with pancreatic disorder, including their potential
pancreatotoxic effects.
Aim:
To assess the prevalence of CAM use in patients with pancreatic
diseases and screen pancreatotoxicity.
Material and methods:
Cross-sectional survey of consecutive
patients seen at a pancreatic disorders outpatient clinic. Data were
collected using a questionnaire regarding demographics, CAM
usage, reasons for CAM use, and respondent experiences of effects
from CAM.
Descriptive statistics were used to analyse the prevalence and the
patterns of CAM use. Fisher test or t-test were used to determine any
association between CAM use, demographics and lifestyle factors.
Results:
108 consecutive patients were enrolled (52% male; mean
age 65+-12,74). The 44% of patients used CAM (44,6% male; mean
age 64+-13) and the 30% for more then 1 year. 47% of patients with
previous acute pancreatitis, 35% with chronic pancreatitis and 41%
with IPMN used CAM. 62% of patients reported advantages with
treatment. CAM users were more often female (55% vs 43 in no
CAM), with higher school degree (42% vs 36% in no-CAM), performed
physical activity more than once a week (51% vs 41% in no-CAM) and
reported anxiety (43% vs 31% in no-CAM) more frequently. However,
none of these differences were statistically significant.
Of the 47 patients using CAM, three reported use of serenoa repens
that has been previously associated with pancreatotoxicity.
Conclusions:
The 44% rate of CAM use in patients with pancreatic
disease is similar or higher to those reported in other GI diseases.
CAM usage is higher in patients with previous AP. 60% of patients
report benefit with CAM. The use seems more frequent in female
with higher education level and “healthier lifestyle”. Patients might
not be aware of potential pancreatotoxicity of CAM, which should be
carefully considered by physicians.
P.02.13
INTRADUCTAL PAPILLARY MUCINOUS NEOPLASMS (IPMNS):
RESULTS OF A THREE-YEAR FOLLOW-UP STUDY
Del Vecchio Blanco G., Tomolillo E.*, Paoluzi O.A., Bevivino G.,
Mannisi E., Fiaschetti V., Pallone F., Monteleone G.
University Tor Vergata, Roma, Italy
Background and aim:
Intraductal papillary mucinous neoplasms
(IPMNs) of the pancreas are neoplasms characterized by ductal
dilation, intraductal papillary growth, and thick mucus secretionis.
The prevalence is high almost 20%, whereby the majority of these
neoplasms are discovered incidentally. Imaging investigations,
such as CT scan, MRI, and endoscopic ultrasound (EUS), allow to
distinguish three subtypes of IPMN according to location, namely
the main duct IPMN [MD-IPMN], branch duct IPMN [BD-IPMN], and
mixed type IPMN. Natural history of IMPN, especially BD-IPMN, is
not well-established and the proper management and follow-up
strategy of BD-IPMN still remain to be fully defined. Aim of the study
was to assess the clinical characteristic and outcome of IPMN.


















