
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e73
The sensitivity, specificity and predictive values (PPPV, NPV) were
evaluated.
Results:
100 patients were enrolled (M: 49), 90 affected by primitive
pancreatic tumour and 10 by non primitive lesions. Among the 90
primitive tumours 72 were ductal adenocarcinoma, 13 mass forming
pancreatitis, 3 IPMN, 1 neuroendocrine carcinoma and one serous
cystoadenoma.
The H&E staining resulted inadeguate in 26 cases (28.9%). After
KRAS mutational analysis among 20/26 cytologic inadeguate cases,
the finding of a KRAS gene point mutation in 10 cases improved the
cytological diagnosis in suspected lesions and the sensitivity of the
procedure (PPV: 93.3%, NPV: 62.5%).
Conclusions:
EUS-FNA procedure with cell-block approach allowed
a correct diagnosis in most of the described cases. Cell-block method
with adjunctive use of ancillary tests such as biomolecular analysis
and immunohistochemical tests provides significant improvement
to the diagnosis in uncertain cytological evaluations.
OC.01.4
EUS PREDICTIVE FACTORS OF RECURRENCE IN PATIENTS WITH
LOCAL ADVANCED RECTAL CANCER
Mannisi E.*, Formica V., Benassi M., Rossi P., Portarena I.,
Nardecchia A., Martano L., Cicchetti S., Sileri P., Paoluzi O.A.,
Giudice E., Sica G., Roselli M., Santoni R., Pallone F., Monteleone G.,
Del Vecchio Blanco G.
Policlinico Tor Vergata, Roma, Italy
Background and aim:
Locally advanced rectal cancer (LARC) remains
a poor outcome disease due to an high rate of pelvic and systemic
recurrence with a negative impact on survival and quality of life of
patients. Several pre-operative prognostic factors have been studied
to select patients with more aggressive disease and high risk of
recurrence. Few data are available regarding the rectal-endoscopic
ultrasound (R-EUS) factors possible related to recurrence. The aim
of this study was to identify R-EUS features of recurrence in patients
with LARC treated with rectal excision after neoadjuvant therapy.
Material and methods:
Consecutive patients with LARC who
underwent neoadjuvant chemotherapy (NACT_RT) and rectal
surgery were studied. Pre and postoperative clinical data were
collected in an electronic database. Computer tomography (CT) and
R-EUS were performed in all patients to stage the disease before
(pre R-EUS) and after (post R-EUS) NACT_RT. Follow-up data on
oncological outcome were retrieved from patient records. Several
clinical and tumor related data were considered such as age, gender,
morphology, distance from anal verge, pre and post-treatment stage,
histological final stage, mucinous phenotype and grading tumor.
During pre e post therapy R-EUS, we assessed: the morphology, the
circumferential rectal wall involvement, the intraluminal tumor
reduction and the residual circumferential rectal wall involvement.
Factors related to recurrence were evaluated by univariate and
multivariate analysis. Disease free survival was estimated using
Kaplan-Meier curve.
Results:
Seventy-four patients were evaluated, 52 male, median age
65,8 years (range 42-82 years). Recurrence was diagnosed in 18 of
74 patients, 7 of which had a local recurrence (9%) and 11 a systemic
recurrence (14%). The one-year recurrence occurred in 6/74 patients
(8%) whereas the remain 12/74 patients (16%) developed recurrence
within the third year. Factors significantly related to recurrence on
univariate analysis were the circumferential involvement evaluated
both in the pre R-EUS than in the post R-EUS (respectively p=0,0418
and p=0,0006), the intraluminal reduction of the tumor after NACT_
RT (p=0,0075), the post R-EUS staging according to TNM (p=0,0237
for N-parameter and p= 0,0329 for T-parameter). As expected the
final histological stage and the grading tumor proven to be related
with high risk of recurrence (respectively p=0,0032 and p=0,027).
Conclusions:
Our data suggest a possible role of restaging R-EUS in
patients with LARC to identify a subgroup of subjects with a major
risk of recurrence and may be used to plan different therapeutic and
follow-up strategy to reduce the recurrence rate.
OC.01.5
ENDOSCOPIC SUBMUCOSAL DISSECTION (ESD) OF LARGE
SUPERFICIAL COLORECTAL NEOPLASMS AT THE DENTATE LINE
OR ILEOCECAL VALVE
Iacopini F.*
1
, Elisei W.
1
, Grossi C.
1
, Montagnese F.
1
, Andrei F.
1
,
Gotoda T.
2
, Saito Y.
3
, Costamagna G.
4
1
Endoscopy Unit, Ospedale S. Giuseppe, Albano L., Rome, Italy,
2
GI &
Endoscopy Unit, Tokyo University, Tokyo, Japan,
3
endoscopy Division,
National Cancer Center Hospital, Tokyo, Japan,
4
surgical Endoscopy
Unit, Università Cattolica, Rome, Italy
Background and aim:
Conventional endoscopic snare resection of
neoplasms at the low rectum is difficult due to the narrowness of the
anal canal, pain sensibility, presence of hemorrhoids; whereas that
of lesions at the ileocecal valve (ICV) due to the ICV itself, difficult
delineation of the tumor border at the ileal mucosa, abundant fat
tissue in the submucosa. Limited data exist for the endoscopic
submucosal dissection (ESD) of these lesions.
Aim:
To assess the efficacy and outcomes of ESD of superficial
neoplasms in the low rectum and ICV.
Material and methods:
Retrospective analysis of prospectively
collected database in a single non academic Western center. From
1.2010 to 7.2015, all consecutive patients underwent ESD for a
superficial neoplasm in the low rectum (within 10 mm from the
dentate line) and over the ICV, and no deep SM invasion (defined
by the Kudo pit pattern V and/or the Sano microcapillary pattern
3B) were included. ESD was performed with the standard technique.
Follow-up was scheduled every 3 or 6 months after piecemeal or
en bloc resection with negative lateral and vertical margins (R0),
respectively. Biopsies were taken regardless the presence of residual
tissue at chromoscopy.
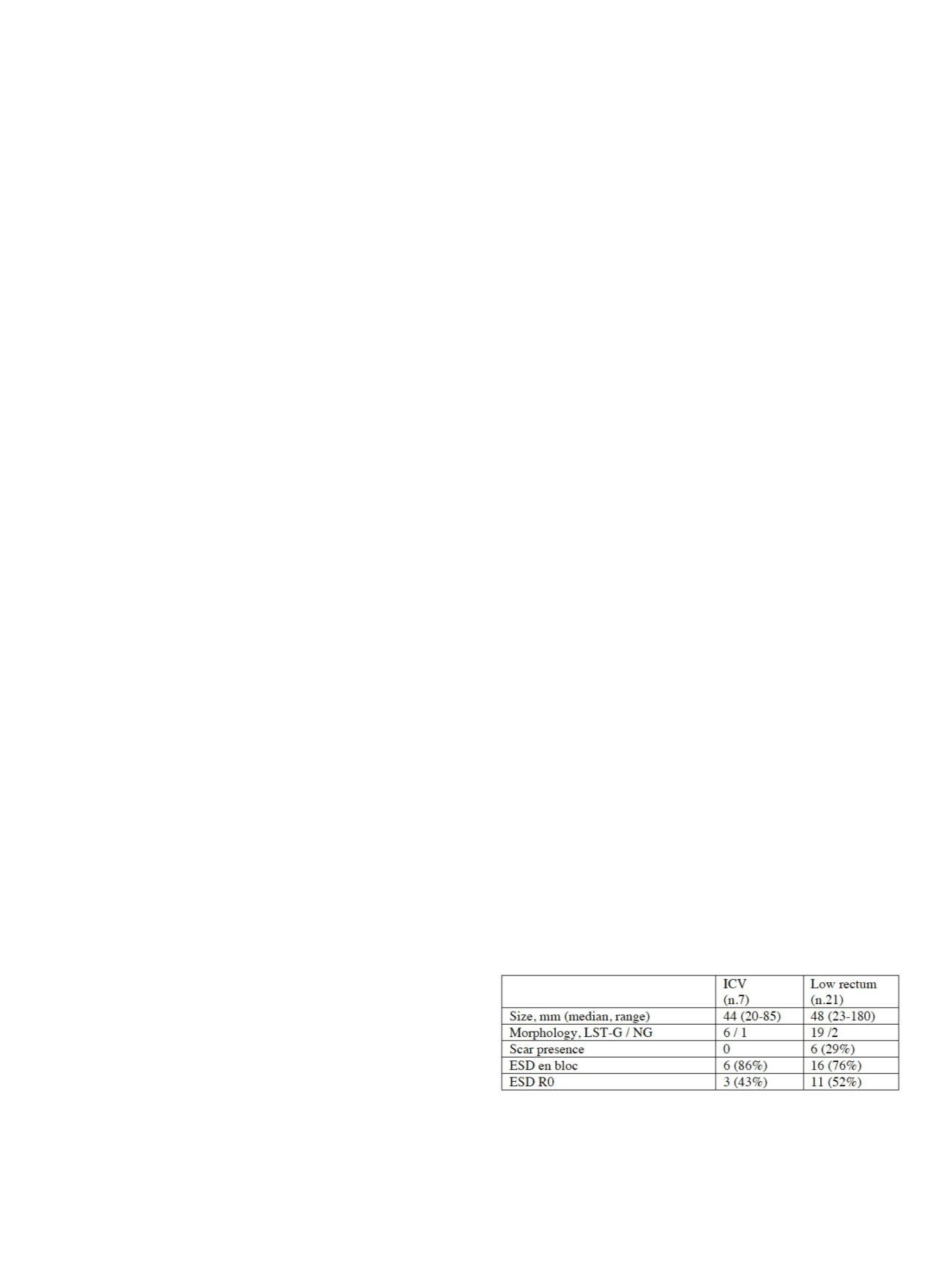
Results:
A total of 7 ICV neoplasms and 21 neoplasms in the low
rectum underwent ESD (Table). Neoplasms in the low rectum
involved the squamous epithelium of the anal canal for at least 50%
of the circumference in 9 (43%) cases. A full involvement of the ICV
lip was observed in 4 (57%) cases, and an extension into the distal
ileum for a median length of 15 mm in 2 (29%) cases. Rectal ESDs
were complicated by a delayed bleeding in 1 case. A curative
resection (also comprising en bloc resections with positive lateral
margins for adenoma without residues at follow-up) was achieved
in 6 (86%) ICV and 14 (67%) rectal lesions. During the follow-up
(median 12 months, range 12-32), a minute area of residual
adenomatous tissue was resected in one (5%) patient underwent
rectal ESD. An asymptomatic substenosis of the anal canal was
observed at digital rectal examination in 2 cases.
Conclusions:
ESD allows en bloc resection of large neoplasms of
the ICV and the low rectum involving the squamous epithelium of
the anal canal. However, the ESD en bloc R0 resection rate is low
due to challenging technical and anatomical aspects that prevent to
perform the mucosal incision far from tumor margins.


















