
e74
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
OC.01.6
UNDERWATER ENDOSCOPIC MUCOSAL RESECTION: THE THIRD
WAY FOR EN BLOC RESECTION OF COLONIC LESIONS?
Amato A.*, Radaelli F., Paggi S., Rondonotti E., Spinzi G.
Ospedale Valduce, Como, Italy
Background and aim:
Underwater endoscopic mucosal resection,
without submucosal injection has been described for removing
large flat colorectal lesions.
Aim of the study was to evaluate the reproducibility of this technique
in terms of ease of implementation, safety and efficacy.
Material and methods:
A prospective observational study of con
secutive underwater endoscopic mucosal resection in a community
hospital was performed.
Results:
From September 2014 to April 2015, twenty-five flat or
sessile colorectal lesions (median size 22.8 mm, range 10-50mm;
18 placed in the right colon) were removed in 25 patients. Two of
the lesions were adenomatous recurrences on scar of prior resection
and one was a recurrence on a surgical anastomosis. The resection
was performed en bloc in 76% of the cases. At the pathological
examination, 14 lesions (56%) had advanced histology and 7 (28%)
were sessile serrated adenomas (two with high-grade dysplasia).
Complete resection was observed in all the lesions removed en bloc.
Intra-procedural bleeding was observed in two cases; both were
managed endoscopically and were uneventful. No major adverse
events occurred.
Conclusions:
Underwater endoscopic mucosal resection appears
to be an easy, safe and effective technique in a community setting.
Further studies tacking the early and late recurrence of this
technique as well as comparing it to traditional mucosal resection
are warranted.
OC.01.7
ENDOSCOPIC MANAGEMENT OF PATIENTS WITH POST-SURGICAL
LEAKS INVOLVING THE GASTROINTESTINAL TRACT. A LARGE CASE
SERIES
Sica M.*
1
, Manta R.
1
, Caruso A.
2
, Cellini C.
2
, Zullo A.
3
, Mirante V.G.
2
,
Frazzoni M.
4
, Tringali A.
1
, Mutignani M.
1
, Conigliaro R.
2
, Galloro G.
5
1
Surgical Digestive Diagnostic and Interventional Endoscopy,
“Niguarda Ca’ Granda Hospital”, Milano, Italy,
2
Gastroenterology
and Endoscopy Unit, “Nuovo S.Agostino” Hospital, Modena,
Italy,
3
Gastroenterology and Digestive Endoscopy, “Nuovo Regina
Margherita” Hospital, Roma, Italy,
4
Digestive Physiopathology
Unit - Baggiovara Hospital, Modena, Italy,
5
Department of Clinical
Medicine and Surgery, Unit of Surgical Digestive Endoscopy, Federico II
University of Naples, Napoli, Italy
Background and aim:
Post-surgical anastomotic leaks often require
a reintervention, are associated with a definite morbidity and
mortality, and with relevant costs. We described the endoscopic
management in a large series of patients with different post-surgical
leaks involving the GI tract.
Material and methods:
This was a retrospective analysis of pros
pectively collected cases with anastomotic leaks managed with
different endoscopic approaches in two endoscopic centres during 5
years. Interventions included: 1) overthe-scope clip (OTCS) position
ing; 2) placement of a covered selfexpanding metal stent (SEMS);
3) fibrin glue injection (Tissucol); and 4) endo-sponge application,
according to both the endoscopic feature and patient’s status.
Results:
A total of 76 patients underwent endoscopic treatment for
an leak either in the upper (47 cases) or lower (29 cases)
gastrointestinal tract, and the approach was successful in 39 (83%)
and 22 (75.9%) patients, respectively, accounting for an overall 80.3%
success rate. Fistula closure was achieved in 84.9% and 78.3% of
patients managed by using a single or a combination of endoscopic
devices. Overall, leak closure failed in 15 (19.7%) patients, and the
surgical approach was successful in all 14 patients who underwent
re-intervention, whilst 1 patient died due to sepsis a 7 days.
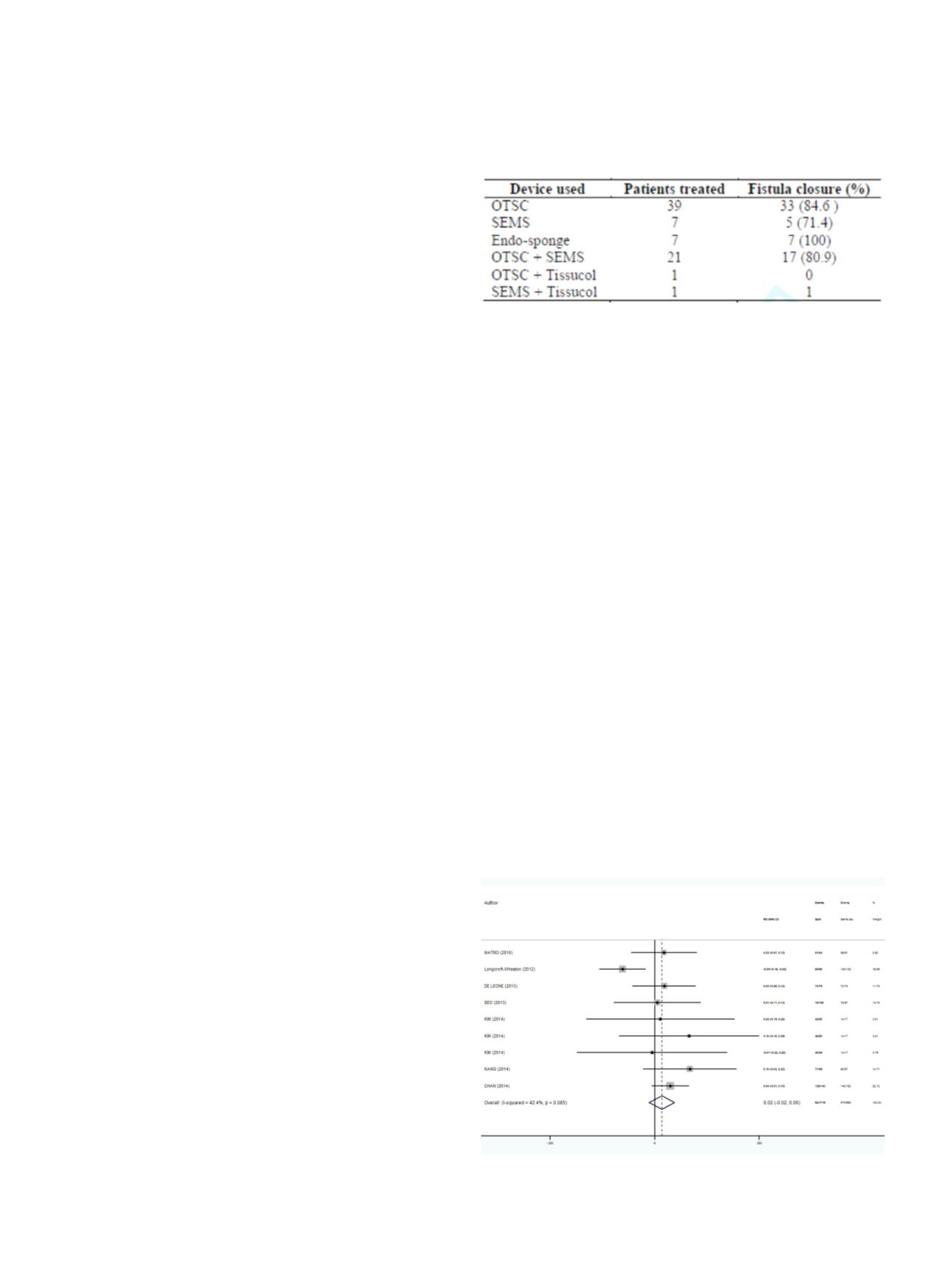
Table 1
Outcome of fistula treatment according to devices used
Conclusions:
Our data suggests that an endoscopic approach is
successful and safe in the majority of patients with anastomotic
GI leaks. Therefore, an endoscopic treatment could be attempted
before resorting in more invasive, costly and risky re-intervention.
OC.01.8
SPLIT VS SAME-DAY REGIMES FOR BOWEL PREPARATION BEFORE
COLONOSCOPY: A META-ANALYSIS OF PUBLISHED STUDIES
Bucci C.*
1
, Marmo R.
2
1
Gastroenterologia, Università di Salerno, Salerno, Italy,
2
Endoscopia,
P.O. L.Curto, Polla (Sa), Italy
Background and aim:
An adequate colon cleaning is essential for
a good quality colonoscopy and the split regimens (S) are actually
considered the standard of care. However, 15-20% of patients
still have an inadequate bowel cleansing after a split preparation.
Recently a new regimen (same-day, SD) in which the purge is
assumed the morning before the colonoscopy has been introduced,
but published studies are underpowered and report controversial
results. Therefore, our aim was to assess the colon cleansing rate of
split vs. same-day regimens.
Material and methods:
Published randomized clinical trials
(1960-2015) comparing S vs. SD preparations in adults undergoing
colonoscopy were selected using MEDLINE, the Cochrane Central
Register of Controlled Trials, clinical trial.gov, ISI Web of Science.
Search terms included bowel, preparation, colon, cleaning,
colonoscopy, same-day and split. Rate difference (RD) of the degree of
colon cleaning between split and same-day was the primary measure
of treatment effect. Compliance (defined as the completion of at least
> 75% of both doses of the purge) and presence of adverse events
(nausea, vomiting, abdominal pain and abdominal discomfort) were
Fig. 1.
Good or excellent grade of colon preparation prior colonoscopy pooled rate
difference between split and same day regimen


















