
e218
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
this anatomical setting can hamper the cannulation of the major
papilla, although a higher incidence of complications has not been
demonstrated. To overcome this issue different tricks have been
proposed, for example the use of a biopsy forceps to change the
position of the papilla in a more favorable position. We reviewed the
outcomes of ERCP in patients with a PAD.
Material and methods:
A single center retrospective analysis
from January 2014 to August 2015. According to its position, the
major papilla was classified in: PED (papilla on the edge of the
diverticulum), PID (papilla in the diverticulum), or NVP (papilla in
the diverticulum but not directly visible). If the standard attempt
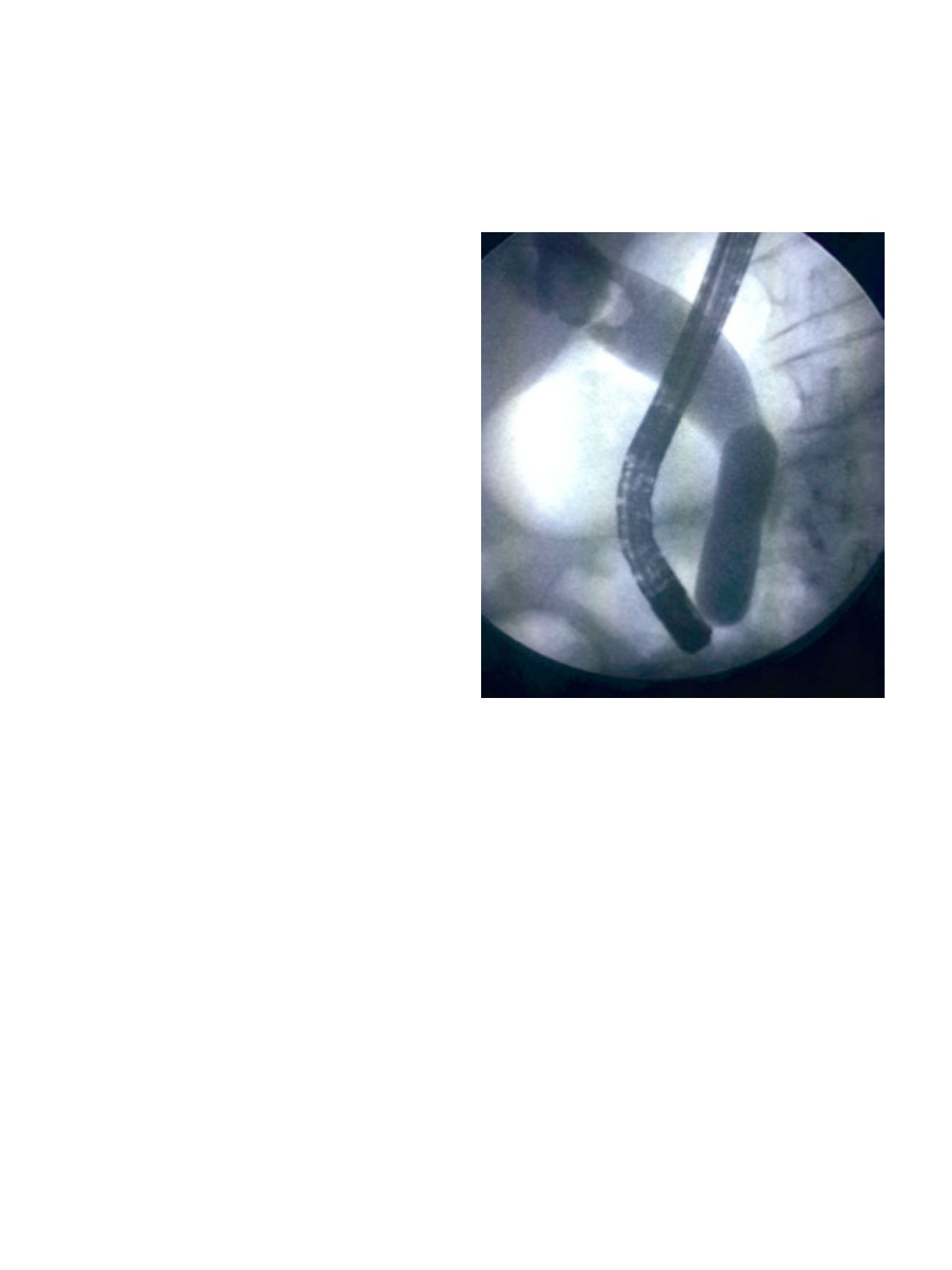
of cannulation with the sphincterotome and the guidewire failed,
a pediatric biopsy forceps was passed in the working channel
of the duodenoscope, parallel to the sphincterotome. Using two
devices at the same time, the mucosa inside the diverticulum was
grasped, shifted or pulled with the forceps in order to get an easier
cannulation with the sphincterotome. We calculated the cannulation
rate and number of complications when the standard technique and
the forceps were used.
Results:
397 ERCPs were reviewed. In 42 cases (11%) a PAD was
identified: 31 patients (74%) had PED, 10 patients (24%) had PID,
1 patient (2%) had NVP. The standard technique was successful in
35 cases (83%), while it failed in 7 (17%); the successive use of the
biopsy forceps get the cannulation in 5 out of 7 patients (2 with PED,
3 with PID); in 2 cases of PED both methods were unsuccessful. After
the standard cannulation a mild post-sphincterotomy bleeding was
seen in 11 out of 35 cases (31%), 2 of witch required epinephrine
injection; on the contrary no complications occurred after the
manipulation of the duodenal diverticulum with the forceps.
Conclusions:
The evidence of a PAD during an ERCP is not rare and
this can prolong or hinder the cannulation of the papilla. In this
study, when the standard technique failed, the use of a biopsy forceps
to change the position of the papilla increased the cannulation rate
from 83% to 95% without additional complications.
P.18.7
ENDOSCOPIC PAPILLARY LARGE BALLOON DILATION FOR THE
REMOVAL OF LARGE STONES IN ELDERLY PATIENTS (80 YEARS
OLD OR OVER)
Zulli C.*, Gargiulo L., Napoli G., Labianca O., Riccio G., Tammaro S.,
Maurano A.
University Hospital San Giovanni di Dio e Ruggi d’Aragona, Ospedale
Amico G. Fucito, Mercato San Severino, Salerno, Italy
Background and aim:
Endoscopic papillary large balloon dilation
[EPLBD] is considered a possible alternative to endoscopic sphinc
terotomy [ES] for the treatment of large bile duct stones (>10mm).
This technique can be used in alternative to ES or following a limited
sphincterotomy [EPLBD + ES] to perform a dilation assisted stone
extraction [DASE]. A recent meta-analysis has shown that ES +
EPLBD technique is a safe technique, with a lower rate of adverse
events than traditional ES. However, little information is available
in elderly patients because of the improved risks of complications,
mainly bleeding or perforation. Particularly, in literature, only one
study investigated the feasibility of EPLBD for large common bile
duct [CBD] stone extraction in elderly patients. We aimed to evaluate
the efficacy and safety of DASE for CBD stone extraction in elderly
patients of 80 years of age or older.
Material and methods:
A total of 22 DASE (EPBLD + ES) procedures
effectuated on elderly patients with evidence of large CBD stones
who underwent ERCPs from January 2014 to September 2015 were
analyzed.
Results:
Median age of patients was 84 (81-93) years, 7 males and
15 females. Thirteen patients had a concomitant duodenal
diverticula. Mean size of stones was 14.07±4.12mm. Cannulation
rate and complete stone extraction rate were 95% (21/22). Wirsung
was cannulated in five procedures and a pancreatic stent (Advanix
Boston Scientific) was placed in two cases. ML was never performed
and use of Dormia was avoided in 31% of cases. Spontaneous stones
expulsion occurred in 7 cases. One patient presented a mild bleeding.
No severe or fatal outcomes were observed. No differences were
observed in procedure results regarding papilla location with
respect to dilation time (30” or 60”).
Conclusions:
This is one of the first studies evaluating efficacy and
safety of DASE for CBD large stones extraction in elderly patients.
Despite the small number of patients, this technique seems to be
safe and effective in patients of 80 years of age or over.
P.18.8
FAMILIAL ADENOMATOUS POLYPOSIS AND EXTRAINTESTINAL
MANIFESTATIONS WITH MALIGNANT POTENTIAL: DIAGNOSTIC
AND THERAPEUTIC APPROACH
Gaiani F.*
1
, Fugazza A.
1
, Bizzarri B.
1
, Nervi G.
1
, De’ Angelis N.
2
1
Gastroenterology and Endoscopy Unit, Parma, PARMA, Italy,
2
Unit of Digestive, Hepato-Pancreato-Biliary Surgery and Liver
Transplantation, Henri Mondor Hospital, AP-HP, Créteil, Paris, France
Background and aim:
Familial Adenomatous Polyposis (FAP) is
characterized by numerous polyps with high malignant potential
in the intestinal tract and high risk of extraintestinal malignancies.
Clinical variants are classic, attenuated (AFAP), MUTYH associated
(MAP) and Gardner syndrome.
Typical extraintestinal manifestations are: Congenital Hypertrophy
of the Retinal Pigment Epithelium, papillary thyroid carcinoma,
osteomas, surrenal glands adenomas, hepatoblastoma, soft tissues
tumors, nasal polyposis.
This study underlines the importance of a multidisciplinary
approach to FAP to allow early detection of malignancies.
Material and methods:
Sixty-three patients were recruited at
Gastroenterology and Endoscopy Unit of University Hospital of
Parma in the period 2004-2015.


















