
e214
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
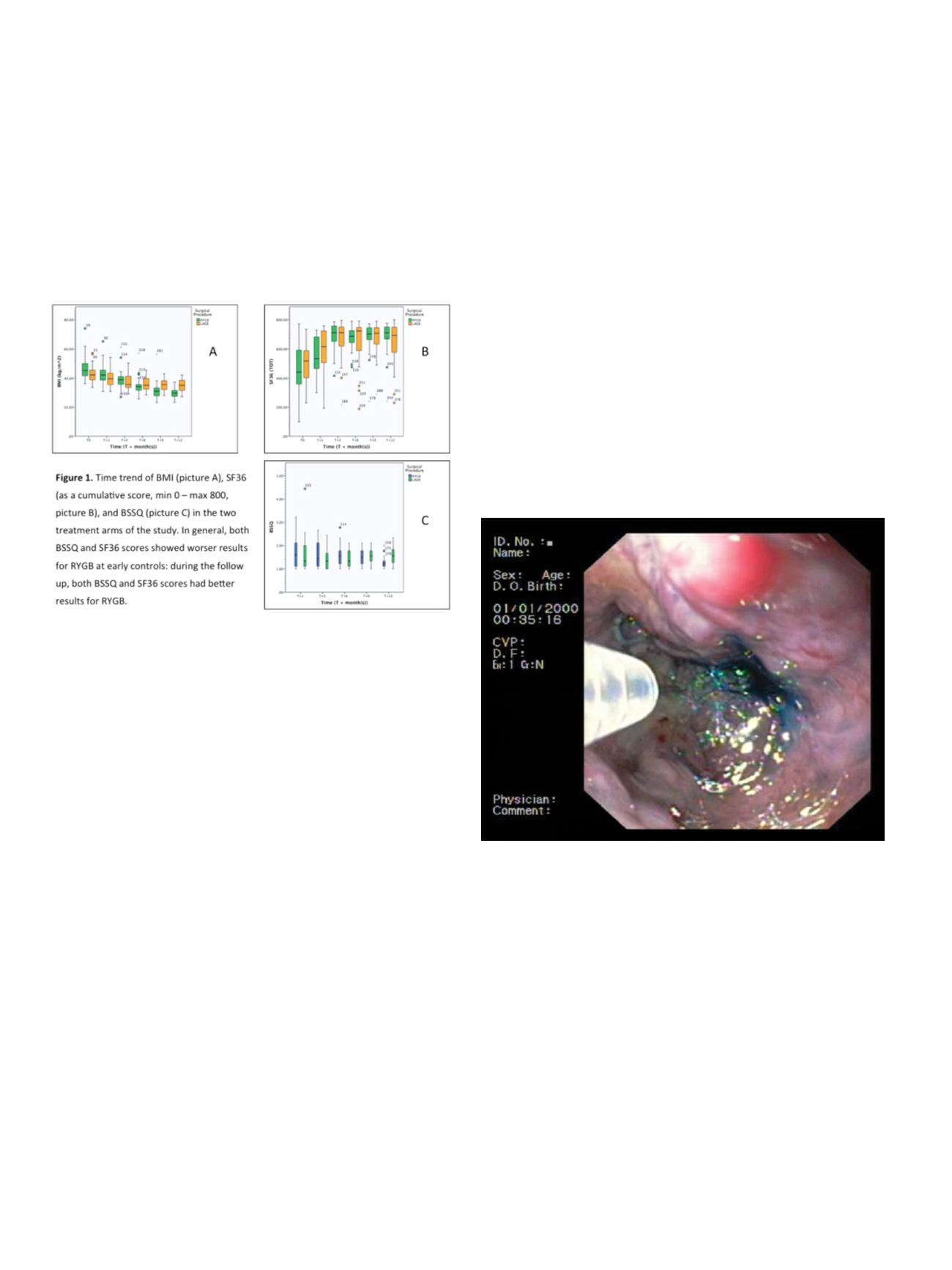
groups; at 12-month control QoL resulted significantly better for
RYGB patients, particularly for SF-36 domains: Role Limitation PH
(p=0.045), Energy Fatigue (p=0.017), General Health (p=0.017), Pain
(p=0.014). Satisfaction for surgery was higher for LAGB at early
controls (6 month), but not statistically significant (p=0.355) and
significantly higher for RYGB at 12 month (p<0.001). Comorbidities
improves both procedures, better in RYGB (p=0.002) especially for
degenerative joint disease (p < 0.0001), similar in LAGB (p= 0.460).
Food dissatisfaction was significantly higher for LAGB, at early
controls (6month, p<0.0001) and late controls (12month, p<0.0001).
Satisfaction for surgery was dipendent to food dissatisfaction (p<
0.001).
Conclusions:
RYGB, compared to LAGB, produces, along with a
higher weight loss and comorbidity resolution, a higher QoL, more
evident starting from 6 month postoperative and more significant at
12 month. The change of QoL, is dependent on type of intervention
(RYGB), independent from BMI preoperative and from changes
of comorbidities during the follow up. Satisfaction intervention,
appears greater in patients undergoing RYGB, directly proportional
to reduction of BMI, negatively to SF-36 and independent from
resolution of comorbidities. An additional parameter for assessing
the effectiveness of the intervention of RYGB, is the best food
dissatisfaction compared to LAGB.
P.17.7
DIGESTIVE BLEEDING IN PEDIATRIC AGE: A SINGLE CENTER
EXPERIENCE
Bizzarri B.*, Gaiani F., Fugazza A., Fornaroli F., Vincenzi F.,
Ghiselli A., De’ Angelis G.L.
Gastroenterology and Endoscopy Unit, Parma, Italy
Background and aim:
Digestive bleedings are important endoscopic
urgencies in paediatric age, with severe morbidity and mortality if
not adequately treated.
They can be divided in high and low, above or under Treitz ligament.
The first ones represents 20% of all gastrointestinal (GI) bleedings in
children, can be variceal or non variceal. In this context, diagnostic
and therapeutic endoscopy is increasingly used.
Aim of this study is to assess clinic, endoscopic presentation, therapy
and complications in children, submitted to endoscopy for acute GI
bleeding.
Material and methods:
In the period 2009-2015, 123 pediatric
patients with acute or acute-recurrent bleeding have been recruited
in our Unit.
After clinic evaluation, patients were stabilized if necessary and
submitted to endoscopy. Active bleedings were treated endoscopi
cally, otherwise medical therapy was started or surgical approach
was required.
In case of negative upper and lower endoscopy, videocapsule
was applied; histology and clinical evaluation for follow up was
scheduled.
Results:
Sixty-three patients were males, median age 4,7 years
(range 2 days-18years). Clinical presentation was: 55 (45%)
hematemesis, 22 (18%) melena, 3(2%) rectal bleeding.
One hundred eleven patients had macroscopic lesions at endoscopy;
78 had sign of recent/active bleeding, of which 1 above superior
oesophageal sphincter, 47 in the upper GI tract (5 variceal, 42 non
variceal), 28 in the lower tract, 2 in both sites.
Endoscopic therapy was necessary in 11 patients (14,1%): 7 had an
upper bleeding, 5 lower. Among variceal bleedings, 2 were band
ligated, 3 were sclerotized with atossisclerol; non variceal bleedings
were treated 1 with adrenaline injection, 1 with adrenaline injection
and clip application.
Lower bleedings were treated endoscopicallywith: 1 clip application,
1 adrenaline injection, 3 polypectomy.
Percentages of relapse of bleeding were: 18% for low, 2% for upper
non variceal, 100% for upper variceal, due to the underlying cause.
Considering all the patients, 90 (73,2%) underwent medical therapy,
2 (1,6%) needed surgery.
Conclusions:
Diagnostic and therapeutic endoscopy demonstrated
to be the gold standard for the management of GI haemorrhages,
with good clinical outcomes if used by expert paediatric endoscopists
experienced in urgencies in Tertiary Care Centers, reducing life
threatening complications.
P.17.8
ENDOSCOPIC SUBMUCOSAL DISSECTION LEARNING CURVE:
EXPERIENCE OF A LARGE VOLUME COLONOSCOPY CRC ITALIAN
SCREENING CENTER
Rosa-rizzotto E.*
1
, Guido E.
1
, Caroli D.
1
, Dupuis A.
1
, Lomele M.
2
,
Rugge M.
2
, Pilati P.
1
, De Lazzari F.
1
1
Ospedale S. Antonio, Padova, Italy,
2
Azienda Ospedaliera, Anatomia
Patologica, Italy
Background and aim:
Endoscopic submucosal dissection (ESD)
is an advanced endoscopic technique that allows for curative
resection of superficial neoplasms in GI tract. The vast majority
of experience and guidelines for ESD resection comes from Japan,


















