
e212
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
defined as the use of hemoclips in the absence of acute bleeding, on
a clean cutting base (no active bleeding, no visible vessel). Delayed
pEMRb (bleeding that required endoscopical consultation) at 30
days from the EMR was reported. We compared the rate of delayed
pEMRb in patients with and without hemoclipping. Good correlation
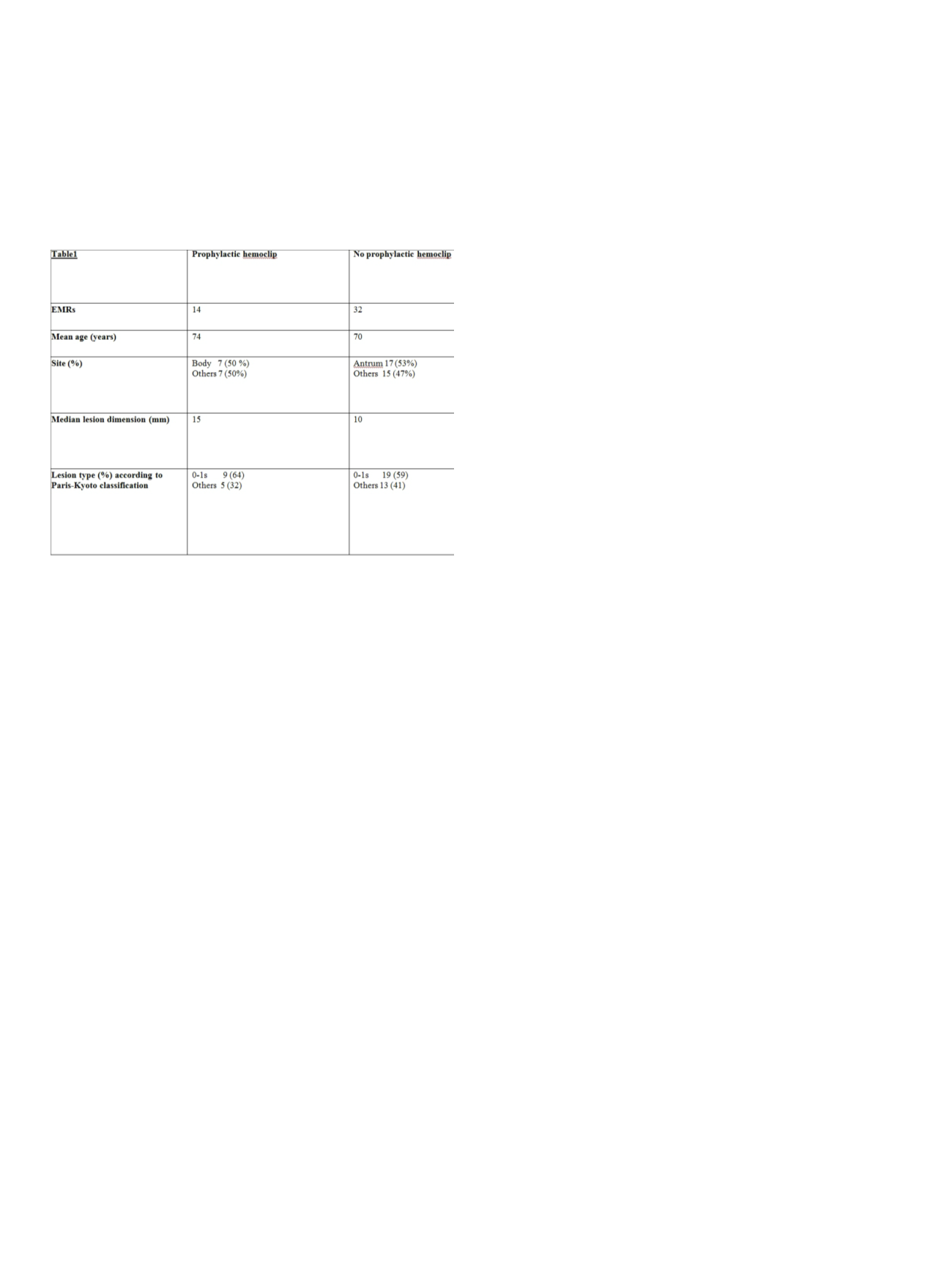
in age, use of anticoagulant/anti-platelet drugs and lesions type.
Median lesion dimension was higher for the group with hemoclips
than the other (table 1). About statistical analysis, a Fisher’s exact
test was used.
Results:
Among all the EMRs, we identified 14 EMRwith prophylactic
hemoclipping and 32 with no hemoclips. Delayed pEMRb occurred
one time in both the groups (7,1% vs 3,1%; p=0,5) with no differences
in the bleeding extent managed endoscopically.
Conclusions:
According to this retrospective single center study,
the risk seems higher in the group where hemoclips were applied.
Although, no significative difference in the occurrence of delayed
pEMRb was found between the two groups of patients. The paucity
of data and the difference in median lesion dimension allow us only
to underline the need for a prospective study to assess the cost-
effectiveness of this prophylactic approach.
P.17.3
COLONOSCOPY IN ELDERLY MORE THAN 80 YEARS OLD: OUR
EXPERIENCE
Labianca O.*, Maurano A.
AOIU San Giovanni di Dio e Ruggi d’Aragona - Gaetano Fucito Hospital
- Digestive Endoscopy Unit, Mercato San Severino (Salerno), Italy
Background and aim:
Colonoscopy (CS) is recognized as the gold
standard for diagnosis of colorectal cancer (CRC) and represents the
diagnostic and therapeutic procedure to more effectively detect and
treat pre-neoplastic lesions. The incidence of CRC increases with
age, and therefore in the elderly population, CS plays a decisive
role in the detection of these cancers, although advanced age can
be a deterrent for its execution. We reviewed our colonoscopy
experience over the last 8- years, in patients beyond 80 years of age,
by assessing the diagnostic yeld, effectiveness and safety.
Material and methods:
A descriptive, retrospective study including
1278 CS performed from January 2008 to September 2015 in
1123 inpatients and outpatients (508 males and 615 females) was
conducted. The mean age was 86,3 years (range 80-98 years). Of
these, 291 patients were subjected to abdominal CT colonography
(virtual colonoscopy). Data recorded included age, indication for
examination, co-morbidities, bowel preparation, colonoscopy report
and therapeutic maneuvers if performed (polypectomies, EMR, and
metallic stent placement). Bowel preparation was made as our unit’s
standard protocol, using PEG lavage solution. CS were considered
complete upon reaching the caecum, and were performed according
to various conscious sedation protocols, and in the presence of
severe co-morbidities with anesthesiologist care.
Results:
The main indications for CS were anemia and
gastrointestinal bleeding, followed by change in bowel habits,
abdominal pain and weight loss. CS was performed completely in
77% (984/1278) of all procedures. Poor bowel preparation (216/294),
intolerance to endoscopic procedure for excessive discomfort
(46/294) and presence of insuperable colonic strictures both benign
and malignant (32/294) precluded complete bowel examination in
23%. Elderly patients have been more likely than younger to have
an abnormal colonoscopy finding. CS revealed a normal bowel in
427 patients (38%), in 265 patients (23,6%) a CRC was diagnosed.
Diverticular diseases and various polyps were observed in 58%,
colitis and vascular diseases in 8%. The risks of CS are generally
associated with the bowel preparation, sedation and the procedure
itself. There were no CS-related deaths, serious complications and
no severe adverse events within 72 hours after the procedure.
Conclusions:
CS is a practicable, effective and quite safe endoscopic
procedure, with an acceptable complications rate, in patients aged
80 years or older, whereas often represents the only therapeutic
option available for these patients. The most common reason for
unsuccessful CS was inadequate bowel preparation. The completion
rate of CS has been good, the diagnostic yield proved high, and there
is a potential benefit for therapy.
P.17.4
PEG IN VERY ELDERLY PATIENTS WITH DEMENTIA: A SAFE
PROCEDURE
Alvisi C.*, Bardone M., Broglia F., Centenara L., Pozzi L., Rovedatti L.,
Strada E., Pratesi S., Bison F., Caserio E., Mantovani E., Dell’Isola D.,
Spadaro S., Ornello C., Carruba L., Vigorelli A., Fumagalli P., Pozzi M.,
Vattiato C., Corazza G.R.
Fondazione IRCCS Policlinico San Matteo, Pavia, Italy
Background and aim:
Percutaneous endoscopic gastrostomy (PEG)
is usually performed for patients with different types of dysphagia
that occurres more frequently in elderly people (> 65 years). Because
of ethical considerations other than procedural and clinical risks in
elderly as well as very elderly people (>80 years), clinicians may deal
with a difficult decision choosing PEG for artificial enteral nutrition.
Material and methods:
We retrospectively analyzed 211 PEG
procedures performed from January 2010 to September 2015. All
procedures were carried out with deep sedation (combination of
intravenous sedative/analgesic anesthesia given by the anesthetist).
Seventy-three patients were older than 80 years (very elderly
people). Major indications for PEG positioning were: non-Alzheimer
non-Parkinson neurogenic dysphagia (37 pts), Parkinson’s disease
(20 pts), head and neck cancer (11 pts), Alzheimer’s disease (1 pt),
miscellaneous (4 pts).
Results:
Pulmonary disease was the most common comorbidity
observed, but did not limit the procedure. No PEG-related
complications were observed, in particular no major complications,
such as buried bumper syndrome, perforation, or bleeding. Only
minimal subcutaeous hematoma were observed in the site of fistula
of a single case, probably due to patient low platelet count.
Conclusions:
The number of very elderly patients with dementia
conditioning dysphagia has increased dramatically over the past few
decades and it could be a medical, ethical and economic problem.
Despite these implications, in our experience PEG is frequently
required for artificial enteral feeding in very elderly people, due
to neurogenic dysphagia. Our data show that in this cathegory of
patients PEG performed under deep sedation is a safe procedure.


















