
e216
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
by double balloon enteroscopy (DBE). After CE, 7 patients (41.2%)
underwent other diagnostic procedure on small bowel (DBE in all
the cases). 16 patients underwent surgical treatment (1 patient
refused it).
Conclusions:
According to previous findings, our data suggest that
CE identify SBT in a small proportion of patients undergoing this
procedure. However, in our series the mean age of patients with SBT
is higher than expected and the main histological type of tumor is
adenocarcinoma, in contrast with previous experiences.
P.18.2
UPPER AND LOWER GASTROINTESTINAL LESIONS OVERLOOKED
AT CONVENTIONAL ENDOSCOPY AND FURTHER DIAGNOSED
WITH SMALL BOWEL CAPSULE ENDOSCOPY: THE CRUCIAL ROLE
OF ENDOSCOPIC EXPERIENCE IN PATIENTS WITH OBSCURE
GASTROINTESTINAL BLEEDING
Moneghini D.*
1
, Missale G.
2
, Minelli L.
1
, Cestari R.
2
1
Chirurgia Endoscopica Digestiva Spedali Civili di Brescia, Brescia,
Italy,
2
Chirurgia Endoscopica Digestiva Università dagli Studi di
Brescia, Brescia, Italy
Background and aim:
The role of small bowel capsule endoscopy
(CE) in the investigation of obscure gastrointestinal bleeding (OGIB)
is well established, with a mean diagnostic yield of 60%. However, in
up to 20% of patients the cause of OGIB is located within the reach
of upper and lower endoscopy. No data are available regarding the
impact of endoscopic experience on the rate of lesions missed by
previous esophagogastroduodenoscopy (EGDS) or ileocolonoscopy
(ICS) and further found with CE. The aim of this series is to clarify
if the experience of the endoscopy units could influence the rate of
overlooked lesions.
Material and methods:
We retrospectively reviewed the charts of
584 patients who underwent CE at Endoscopy Unit between October
2008 and March 2015 for OGIB. The CE-derived data are recorded
and analyzed in terms of non-small-bowel CE findings (gastric,
duodenal and colonic lesions) overlooked at previous upper and
lower endoscopy. The type of endoscopic units who performed
the conventional endoscopy (tertiary referral centres or primary
level centres) and the respective lesions miss rate was recorded.
The Given M2A video capsule system (Pillcam; Given Imaging Ltd,
Yoqneam, Israel) was used.
Results:
547 patients were enrolled for the final investigation (41
cases were excluded from further analysis because of the capsule
did not reach the colon). In 35 patients (6.4%) one or more lesions
previously missed by conventional endoscopy were diagnosed at CE.
20 of these 35 cases were males. The mean age was 72.8 years (range
51-89). 77.1% of lesions were overlooked at primary level endoscopy
units; 22.9% at tertiary level units (p<0.01). The overlooked lesions
are reported in the table according to the type of endoscopic centre.
The most frequently missed lesions were located in stomach and
duodenum (66.6%); primary centres missed lesions mostly during
EGDS (71.4%); tertiary centres miss lesions during EGDS and ICS
equally. Both types of centres can miss neoplasias (66.6% at primary
centres): tertiary centre overlooked a gastric GIST (gastrointestinal
stromal tumor); primary centres overlooked a non invasive
intraepithelial gastric haemorrhagic neoplasia and an ascending
colon adenocarcinoma.
Conclusions:
Our results suggest that endoscopic experience, in
terms of number of referral patients, can significantly reduce the
miss rate of lesions located in upper or lower gastrointestinal tract,
avoiding unhelpful CE.
P.18.3
EARLY WAKE UP, ONE DAY LOW FIBER DIET: SPLIT BOWEL EVEN
FOR PATIENTS UNDERGOING COLONOSCOPY EARLY IN THE
MORNING. A REAL LIFE EXPERIENCE
Checchin D.*
1
, Ntakirutimana E.
1
, Cristofori C.
1
, Viaro T.
1
, Rostello A.
1
,
Inturri P.
1
, Costa P.
2
, Bulighin G.
1
1
UOC di Gastroenterologia ULSS20, San Bonifacio, Verona, Italy,
2
UOC
di Medicina del Territorio ULSS20, Verona, Italy
Background and aim:
Bowel preparation is crucial for colonoscopy
outcome. Split preparation is the gold standard but its application
among subjects undergoing colonoscopy during the first part of
morning endoscopy sessions is still object of discussion for reasons
of compliance.
Since 1st January 2015 we have extended split prep with just one
day of low fiber diet also to subjects undergoing colonoscopy
before 11.00 AM despite the need for an early wake up the day of
colonoscopy. Previous version included low fiber diet for 3 days and
4 l prep the day before colonoscopy without the need for night-time
bowel cleaning. Aim of this study was to compare colonoscopy per
outcome before and after data sheet update.
Material and methods:
The 9 months before the new regimen
introduction (Pre) and the 9 months after new regimen introduction
(Post) were compared. Inpatients were excluded. Data of bowel
preparation were prospectively collected and colonoscopies were
performed by the same team of five gastroenterologists.
A modified Aronchick scale including 4 grades was used to assess
bowel preparation. Chi square test was used when appropriated.
Significance was set at p<0.05.
Results:
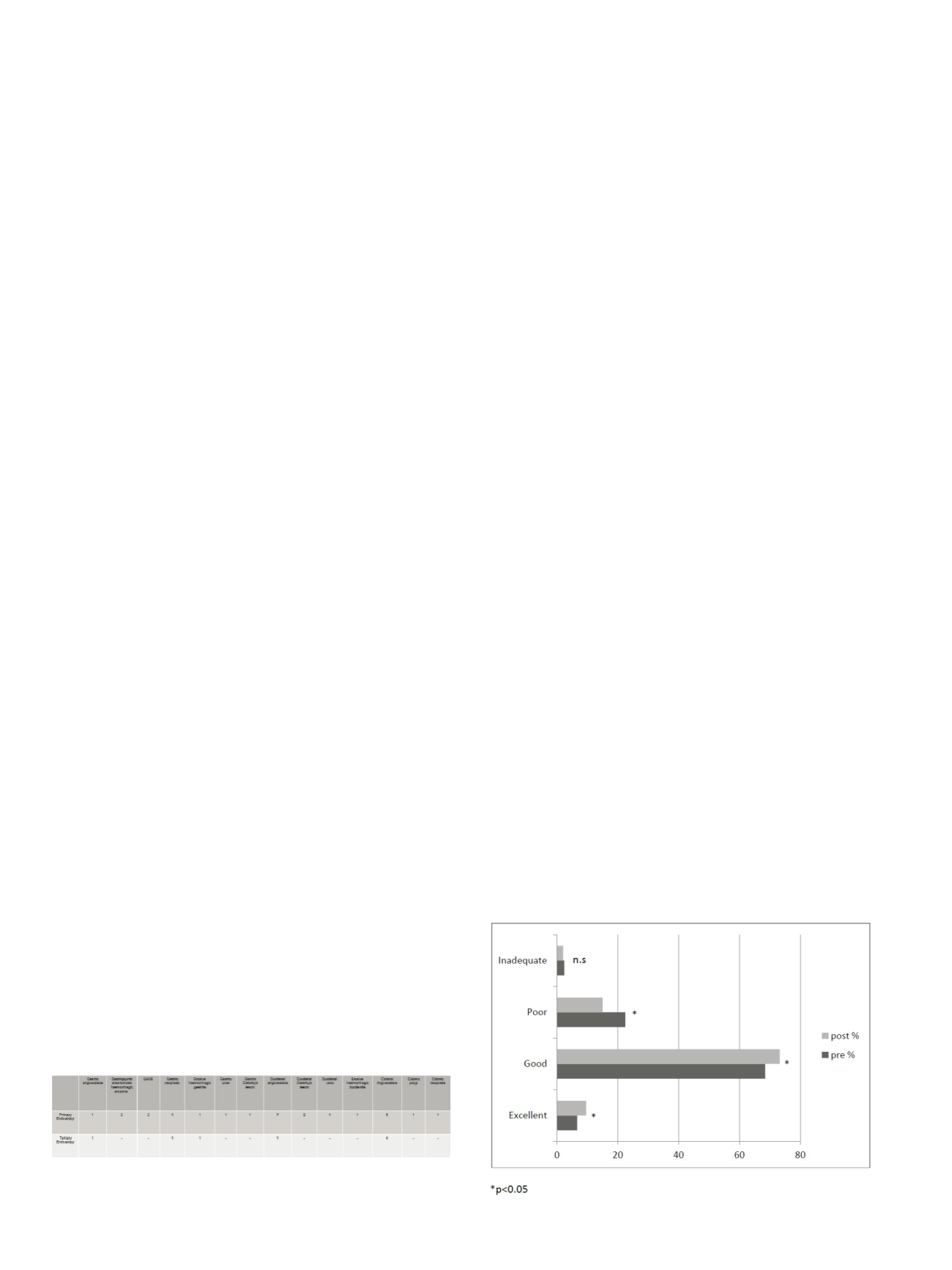
Pre period included 1608 colonoscopies, and post 2134.
After extension of the split regimen to all colonoscopies, the rate of
excellent preparations increased by/to 45% (206/2134; 9.65% vs
107/1608 6,65% p<0.005); the rate of good preparations increased
by/to 6% (1563/2134; 73% vs 1101/1608 68.4%; p<0.05); the rate of
poor preparation decreased of by/to32% (321/2134; 15% vs 361/1608
22%; p<0.05) but the difference among rates of inadequate
preparation wasn’t significant (44/2134; 2.0% vs 39/1608 2,4% n.s.).
The rate of repeat colonoscopies due to inadequate preparation was
significantly lower (400/1608; 24,8% vs 365/2134 17,1% p<0.001).
Data suggest that compliance was good even if early wake up was
necessary. The rate of subjects with completely inadequate
preparations was the same maybe because of general non acceptance
of preparation procedure.


















