
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e207
P.16.4
ENDOSCOPIC ULTRASOUND-GUIDED TRANSMURAL STENTING
FOR GALLBLADDER DRAINAGE IN HIGH RISK PATIENTS WITH
ACUTE CHOLECYSTITIS: A SYSTEMATIC REVIEW AND POOLED
ANALYSIS
Anderloni A.*
1
, Buda A.
2
, Vieceli F.
2
, Khashab M.A.
3
, Hassan C.
4
,
Repici A.
1
1
Humanitas Research Hospital, Milano, Italy,
2
Ospedale Santa Maria
del Prato, Feltre, Italy,
3
The Johns Hopkins Medical Institutions,
Baltimore, MD, United States,
4
Ospedale Nuovo Regina Margherita,
Roma, Italy
Background and aim:
Endoscopic ultrasound-guided transmural
stenting for gallbladder drainage is an emerging alternative for the
treatment of acute cholecystitis in high risk surgical patients. A
variety of stents have been described, including plastic stents, self-
expandable metal stents (SEMSs), and lumen-apposing metal stents
(LAMSs). LAMSs represent the only specifically designed stent for
transmural gallbladder drainage. A systematic reviewwas performed
to evaluate the feasibility and efficacy of EUS-guided drainage (EUS-
GBD) in acute cholecystitis using different type of stents.
Material and methods:
A computer-assisted literature search up
to September 2015 was performed using two electronic databases,
MEDLINE and Embase. Search terms included MeSH and non-
MeSH terms relating to acute cholecystitis, gallbladder drainage,
endoscopic gallbladder drainage, endoscopic ultrasound gallbladder
drainage, alone or in combination. Additional articles were retrieved
by hand-searching from references of relevant studies. Pooled
technical, clinical and adverse event rates were estimated using all
included studies.
Results:
Twenty-one studies met the inclusion criteria and the
eligible cases were 166. The overall technical success rate, clinical
success rate and frequency of adverse events were 95.8%, 93.4%
and 12.0%, respectively. The technical success rate was 100% using
plastic stents, 98.6% using SEMSs and 91.5% using LAMSs. The
clinical success rate was 100%, 94.5% and 90.1% after the deployment
of plastic stents, SEMSs and LAMSs respectively. The frequency of
adverse events was 18.2% using plastic stents, 12.3% using SEMSs
and 9.9% using LAMSs.
Conclusions:
Among the different drainage approaches in the non-
surgical management of acute cholecystitis, EUS-guided transmural
stenting for gallbladder drainage appears to be feasible, safe and
effective. LAMSs seem to have high potentials in terms of efficacy
and safety, although further prospective studies are needed.
P.16.5
TRANSORAL OUTLET REDUCTION FOR THERAPY OF WEIGHT
REGAIN AFTER GASTRIC BYPASS
Boskoski I.*, Familiari P., Tringali A., Landi R., Perri V.,
Costamagna G.
Ospedalle Gemelli, Roma, Italy
Background and aim:
Enlargement of gastrojejunal anastomosis
aperture is associated with weight regain in patients with Roux-
en-Y gastric bypass (RYGB). Endoscopic transoral outlet reduction
(TORe) has proven safe and effective for treatment of weight regain.
The objective of this study was to evaluate the results of endoscopic
outlet reduction in single Italian center.
Material and methods:
The series included consecutive post-RYGB
patients with weight regain and enlarged gastrojejunal anastomosis
aperture (>15 mm). Endoscopic reduction was performed with a
full-thickness endoscopic suturing device at our endoscopy unit.
Results:
Nineteen patients who had regained weight after gastric
bypass (BMI > 35) underwent TORe from January to September 2015.
Baseline mean BMI was 36.8 (range 33-43.6) and weight was 104.5
kg (range 85-131). The procedure was done with the Overstitch
device (Apollo Endosurgery) and Olympus double channel operative
endoscope. An Overtube (US Endoscopy) was placed before the
procedure in all patients. Before suturing the outlet rims were
cauterized with pulsed pulsed Argon Plasma (ERBE Vio 200) on 40
Watts in all patients. Mean procedure time was 35 minutes (range
15-60) and a mean number of 2.3 stitches per patient were placed
(range 2-4) on the level of the gastric outlet. After suturing the
patency of the new redone outlet was tested with standard
gastroscope. There were three (15.7%) complications of which two
were mild (one intraoperative bleeding that arrested spontaneously
and fever due to small retrogastric collection treated with
antibiotics), while one patient (5.2%) had gastric perforation that
required urgent surgery. Mean hospital stay was 2.8 days (range
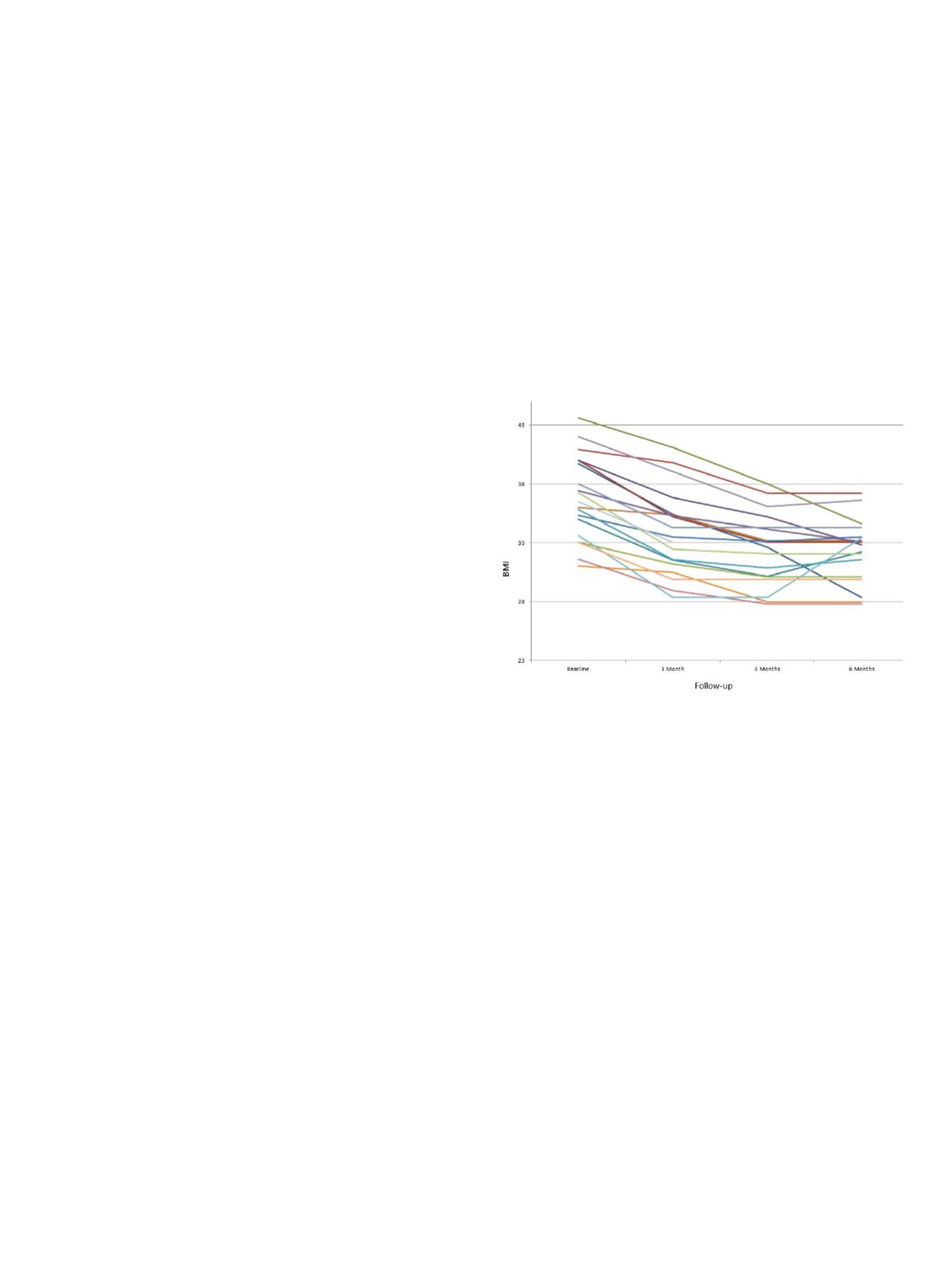
2-10). Telephonic follow-up was done at 1, 3 and 6 months. Mean
BMI at 1 month follow-up was 33.8, at 3 months was 32.4 while at 6
months was 32.3. Figure 1 shows the BMI during follow-up for each
patient.
Conclusions:
In our experience TORe was safe and effective
procedure in patients with weight regain after RYGB. Longer follow-
up is needed to establish the durability of these results. Further
studies are however needed to better understand the role of TORe
after RYGB and the proper selection of patients.
P.16.6
ENDOSCOPIC TREATMENT WITH SELF EXPANDABLE METAL
STENT OF NEOPLASTIC COLONIC STRICTURES
Bucciero F.*, Fonte G., Manetti R., Talamucci L., Naspetti R.
AOU Careggi, Firenze, Italy
Background and aim:
To evaluate the clinical efficacy of endoscopic
treatment of neoplastic colonic strictures with self expandable
metal stents (SEMS) positioned with palliative intent or “bridge to
surgery”.
Material and methods:
We placed SEMS for the treatment of
neoplastic stenosis from July 2009 to April 2015 c/o the Digestive
Endoscopy and Surgery Rooms of AOU Careggi in Florence.
Results:
We placed 90 SEMS for the treatment of neoplastic stenosis
from July 2009 to April 2015 c/o the Digestive Endoscopy and
Surgery Rooms of AOU Careggi in Florence.
Patients were 85, including 42 women and 43 men with an average
age of 76 years.
45 stents were placed as “bridge to surgery” and elective surgery
was performed after 30 days (range 9-180 days), 45 stents were
placed with palliative intent.


















