
e204
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
hospital stay in variceal bleeders (VB) vs. non-variceal bleeders (VB).
Pre specified death causes were registered.
Results:
A total of 2,628 patients were included, of which 549 (20.9%)
had liver cirrhosis. The bleeding source was variceal in 404 (73.6%)
and non-variceal in 145 (26.4%) patients. Characteristics of the 2
groups are described in table 1. Among the VB, the source of AUGIB
was oesophageal in 304 (80.2%) and gastric in 66 (16.3%), while
among the NVB the source was portal hypertensive gastropathy in
33.1%, a gastric or duodenal ulcer in 20%, a vascular lesions in 14.5%
or a gastroduodenal erosions in 13.1%. 265 (65.6%) VB patients were
transfused vs 81 (55.9%) of the NVB (p< 0.04). Six patients in VB
group and one in NVB group were treated with TIPS (1.5% vs. 0.7%).
Overall, recurrent bleeding, need for surgery, 45-day mortality
did not differ between groups. The most frequent causes of death
were liver failure (34%), multi organ failure (24%) and respiratory
insufficiency (12%) among the VB, and multi organ failure (42.8%)
respiratory insufficiency (14.3%) and sepsis (7.4%) among the NVB.
The death causes were judged not directly linked to the blood loss in
77% and in 82% of VB and NVB.
Table
Variceal bleeders Non-variceal bleeders
(VB, n = 404)
(NVB, n= 145)
P
Gender (male, %)
68.5 %
67.5 %
0.24
Age (mean ± SD)
63.6 ± 12.1
62.2 ± 14.8 0.35
Child score (mean ± SD)
8.1 ± 3.06
7.8 ± 2.2
0.21
Haemoglobin value (mean ± SD)
8.9 ± 2.0
9.3 ± 2.4
0.08
Hemodynamic instability (%)
8.9%
7.3%
0.56
Use of aspirin (%)
6.9%
6.2%
0.77
Use of NSAIDS (%)
5.7%
8.3%
0.27
Hematemesis as clinical presentation (%) 81.7%
51%
<
0.0001
Hepatocellular carcinoma (%)
28.3%
20.8%
0.08
Transfusion (%)
65.6%
55.9%
0.02
Rebleeding (%)
9.2%
5.5%
0.17
Death
12.4%
11.7%
0.84
Conclusions:
Recurrent bleeding, need for TIPS or surgery are
infrequent events in our cohort. Transfusions are more frequently
prescribed in variceal bleeders. Mortality due to variceal or non-
variceal bleeding is similar, as the great majority of mortality was
unrelated to blood loss per se.
P.15.9
TRANSFUSION STRATEGY AND DEATH RISK IN PATIENTS
WITH ACUTE NON VARICEAL UPPER GASTRO INTESTINAL
BLEEDING (NV-UGIB) IN ITALY: A PROSPECTIVE MULTICENTER
OBSERVATIONAL STUDY
Marmo R.*, Soncini M., Cipolletta L., Parente F., Paterlini A.,
Bennato R., Cipolletta F., Orsini L., Bargiggia S., Cesaro P., Bizzotto A.,
Dell’Era A., Germanà B., Cavallaro L.G., Riccioni M.E., Marmo C.,
Tortora A., Segato S., Parravicini M., Purita L., Chirico A., Spinzi G.,
Imperiali G., Maringhi A., Boarino V., Bresci G., Metrangolo S.,
Bucci C., Baldassarre G., Franceschi M., Soncini M., Nucci A.,
De Nigris F., Masci E., Marin R., Antoniazzi S., Ferraris L., Repici A.,
Andreloni A., Bianco M.A., Rotondano G., De Matthaeis M., Lauri A.,
De Fanis C., Borgheresi P., De Stefano S., Lamanda R., Furio L.,
Russo A., Di Giorgio P., Politi F., Pumpo R., Triossi O., Coccia G.,
Montalbano L.M., Zagari R.M., Balzano A., Buscarini E., Conte D.,
D’Amico G., Di Giulio E., Gasparini P., De Franchis R.
Gruppo Italiano Studio Emorragia Digestiva, Rome, Italy
Background and aim:
Acute non-variceal upper gastrointestinal
bleeding (NV-UGIB) is a frequent indication for hospital admission
and blood transfusions. A liberal use of blood supplies may affect
the mortality, but studies on the correct strategy for transfusion of
patients with hemoglobin between 7 and 9 g/dL are inconclusive.
Aim:
we evaluated the impact of transfusion strategies on death risk
in patients with NV-UGIB.
Material and methods:
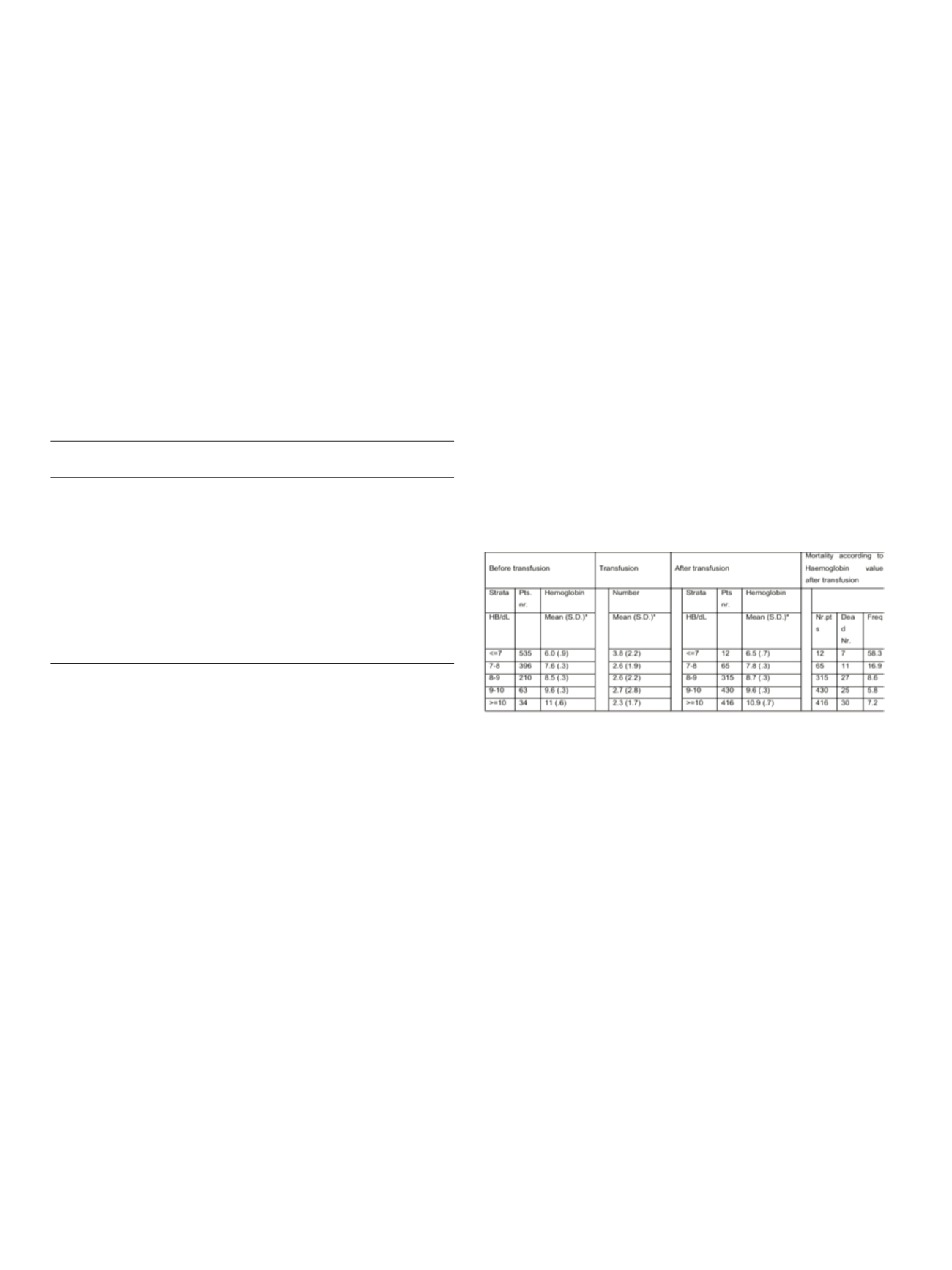
Prospective data on patients admitted for
NV-UGIB were collected from January 2014 to September 2015. 30-
day mortality and transfusion strategy were the primary outcomes.
Transfusion strategy definitions: “restrictive” if the patient was
transfused for hemoglobin (Hb) levels ≤7g/dL; “not justified” for
Hb levels from 7 to 9gr/dL; “liberal” for Hb levels ≥9gr/dL; “not
indicated” for Hb levels ≥10gr/dL.
Results:
2,191 NV-UGIB patients were included (mean age 69.2,
67.1% males). Comorbidities were present in 75.8%. At admission,
meanHb valuewas 9.3±2.6 and7.2%of the patients hadhemodynamic
instability. Overall, half of the patients (56.4%) were transfused,
receiving a mean of 3.1 blood units, with a mortality rate of 5.8%.
Need for transfusions impacted on mortality, being statistically
different between transfused and non-transfused patients (8.1% vs.
2.9% p<0.000), and the death risk varies considerably within the Hb
value (tab.1). 43% of the patients had a restrictive transfusion
strategy while 7.8% received a liberal. In the restrictive group, mean
infusion of 3.8 RBCs units increased Hb value from ≤7 g/dL to 7.8 gr/
dL in 98% of patients; in those with persistent low Hb levels, death
occurred in 58%. In the not justified group, after the administration
of a mean of 2.6 units, the Hb did not change substantially in 65 pts
and 16.9% of them died. Both in the restrictive and in the not justified
group, when Hb increased over 9 g/dL, we observed a substantial
decrease in mortality rate, fluctuating between 5.8% and 8.6%
(p<0.13).
Conclusions:
The “restrictive” transfusion strategy was adopted in
43% of patients with NV-UGIB while the liberal was adopted only in
a minority of patients with no effect the mortality rate. Reassessing
Hb concentration during transfusions and an appropriate transfusion
strategy could reduce an over-utilization of RBC as a substantial
number of transfusions were administered without indication.
P.15.10
ENDOSCOPIC TREATMENT OF ANASTOMOTIC STENOSIS AFTER
INTESTINAL RESECTION FOR DEEP ENDOMETRIOSIS: A SINGLE
CENTER’S EXPERIENCE
Orlandi S.*, Variola A., Benini M., Rossini R., Barugola G.,
Geccherle A., Ruffo G., Bocus P.
Sacro Cuore Don Calabria, Negrar, Italy
Background and aim:
Endometriosis is a very complicated
multivisceral disease. Intestinal resection for deep endometriosis
is associated with many complications, the most frequent is
anastomotic stenosis. Our experience shows that for this kind of
complication endoscopic approach is safe and feasible.
Material and methods:
We collected from our database the single
center experience about deep endometriosis surgery (data from
2010 until 2014).
Of the 1548 female patients who underwent intestinal resection
for deep endometriosis, we studied the patients affected by post-
operative anastomotic stenosis. We evaluated the surgical features


















