
e202
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
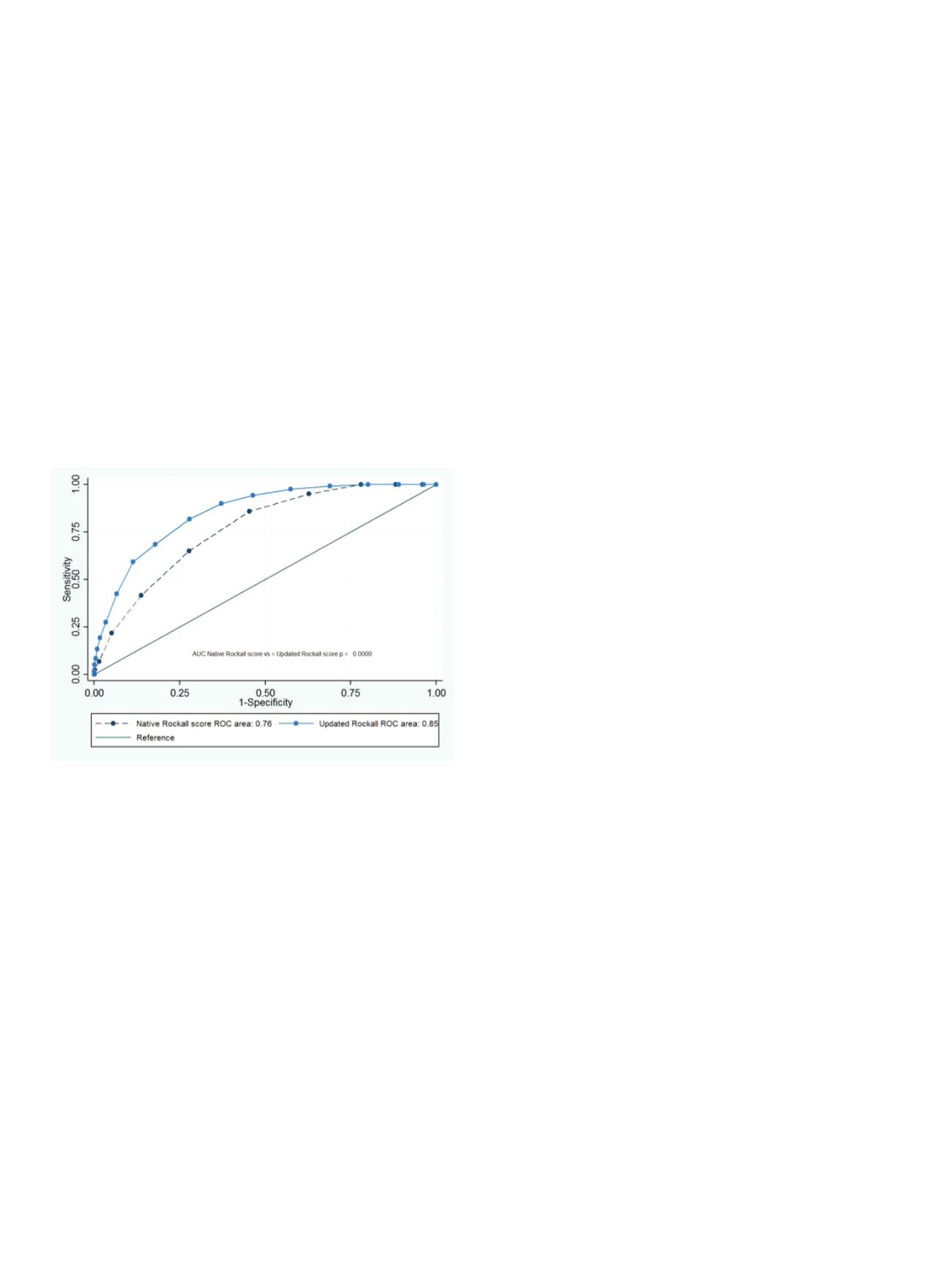
outcome was 30-day mortality. We integrated the traditional risk
factors for mortality considered in the Rockall score with those
more recently recognized in the literature, e.g. inpatients bleeding,
endoscopic treatment failure, comorbidities severity (evaluated by
American Society of Anaesthesiologists physical status classification,
or ASA score), rebleeding and need for surgery. Statistics: the
performance yield of prognostic scores was assessed by comparing
the ROC curves
Results:
A total of 2,191 patients with ANV-UGIB were included
(mean age 69.2, 67.1% male). Comorbidities were present in 75.8%
and were judged as severe (ASA score 3-4) in 34.7% patients. At
admission, 7.2% of the patients had hemodynamic instability and
inpatient bleeding occurred in 410 (19.9%). Rebleeding and need for
surgery occurred respectively in 124 (5.6%) and 90 (4.1%) patients
with an overall mortality of 5.8%. in those patients, the native Rockall
score had a performance of 76% [AUC= 0.76 (0.73 to 0.80], while
when we integrated additional risk factors, the updated Rockall
provide a better performance [AUC= 0.85 (0.82 to 0.88) p <0.000,
Figure 1]. Compared the native score, the new Rockall has a better
sensitivity for death risk between 5 to 7 points (94.2% vs. 65.0%) and
an implemented sensitivity for score ≥ 8 points (81.7% vs. 21.7%,
p<0.000).
Conclusions:
In ANV-UGIB patients, different events could occur
during hospital stay, which in turn can increase the death risk.
Unfortunately, those are not considered during the initial clinical
triage of those patients. Our data show that when the traditional
Rockall score is implemented with new risk factors, the accuracy and
sensitivity are implemented, thus allowing a better identification of
patients with a higher mortality rate.
P.15.4
BLACK ESOPHAGUS: AN UNCOMMON CAUSE OF NON VARICEAL
UPPER GI BLEEDING
Massidda M.*
1
, Gaffuri N.
1
, Bettoni E.
1
, Genco C.
2
1
Istituto Clinico Humanitas Gavazzeni, Bergamo, Italy,
2
Istituto
Europeo Oncologico, Milano, Italy
Background and aim:
Black esophagus or acute esophageal necrosis
(AEN) is a rare cause of acute upper gastrointestinal bleeding
(AUGIB) characterized by circumferential black appearance of distal
esophageal mucosa that stops abruptly at gastroesophageal junction
(GEJ). It is diagnosed in elderly men with multiple comorbities and
younger adults with history of alcohol consumption. Etiology take
into account an initial ischemic damage and a topical injury that
can lead to diminished mucosal defense and compromission of the
intrinsic repair mechanisms. We report a case of AUGIB due to AEN.
Material and methods:
A 67-year-old man presented to the
emergency department with hematemesis after three days of fever,
right hypochondriac pain and vomiting. He reported moderate
recent alcohol consumption but no NSAIDs abuse. Laboratory
evaluation revealed conjugated hyperbilirubinemia with cholestasis,
hemoglobin 15.6 g/dL which decreased to 13 g/dl six hours later;
glycemia 467 mg/dl; BUN 241 mg/dL. On presentation, he was given
an iv bolus of proton pump inhibitor (PPI) 80 mg followed by an iv
PPI drip at 8 mg/h. A CT scan showed gallbladder, common bile duct
and intrahepatic gallstones with dilation of biliary tree.
Results:
An urgent upper endoscopy (EGD) revealed striking
diffuse circumferential black discoloration of the middle and
distal esophagus with abrupt interruption at the GEJ and no
active bleeding. Endoscopic biopsies were deferred and no further
endoscopic intervention was required. The patient was kept nil-
per-os with iv hydration, insulin and antibiotic therapy. Three days
after admission a second endoscopic look revealed white-yellow
circumferential exudates in the middle and distal esophagus. After
ERCP and cholecystectomy he progressively recovered without any
complication. He started soft diet at day 7 and was discharged in
good clinical conditions one week later.
Conclusions:
AEN is a rare cause (prevalence 0.001-0.2%) of AUGIB
with multifactorial etiology. Endoscopic appearance is diagnostic
and histologic confirmation is not warranted unless other etiologies
are suspected. Management consists of treatment of the underlying
diseases, fasting and high dose PPI. Antimicrobic therapy is indicated
only when infections are suspected. Mortality ranges from 13 to 35%
and esophageal perforation is reported up to 7% of cases. About
40% of patients develop progressive dysphagia due to esophageal
strictures. In conclusion, although AEN is a rare condition it should
be considered and mentioned on international guidelines as a
possible cause of AUGIB.
P.15.5
GUIDE WIRE ASSISTED CANNULATION OF MINOR PAPILLA IN
PANCREAS DIVISUM: OUR EXPERIENCE
Sica M.*, Mutignani M., Forti E., Pugliese F., Tringali A., Manta R.
Surgical Digestive Diagnostic and Interventional Endoscopy, “Niguarda
Ca’ Granda Hospital”, Milano, Italy
Background and aim:
The minor papilla cannulation is a challenging
procedure with an high rate failure in literature (20%)*. We describe
our experience of endotherapy in patients with pancreas divisum
affected by symptomatic pancreatic diseases.
Material and methods:
From April 2012 to October 2013 14 patients
with pancreas divisum affected by symptomatic diseases underwent
ERCP using a minor papilla approach. We retrospectively evaluated
technical results at first attempt and early complications as well.
Results:
In patients with a diagnosis of pancreas divisum (11/14)
we approroached directly to the minor papilla with a double lume
sphincterotome (Mini-Tome, Cook) and a 0.018 fr hydrophilic guide
wire without contrast injection (WIRE-GUIDE CANNULATION), then
we performed sphincterotomy and plastic stent placement (calibre
5, 8.5 or 10 Fr).
The minor papilla cannulation was achieved in 13 of 14 patients
(92.8%) at first attempt, in one case, after unsuccessful pre cut, we
repeated ERCP the next day and we got a successful cannulation
after secretin’s injection for a better visualization of duct’s opening.
Endoscopic minor papillotomy (EMP) was performed in 13 of 14
patients using a sphincterotome (Mini-Tome, Cook). Pancreatic stent
was placed in 92.8% of cases. In 3 cases we need to remove the stent
repeating the endoscopy, in the others we observed a spontaneuos
migration.


















