
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e197
skipped the other drugs, and 10% were non-adherent to mesalazine
or to IMMs because of worries about adverse events.
Conclusions:
IBD patients of our series showed a scarce compliance
to long term therapy particularly when in clinical remission or
when they consider a drug less effective than other (mesalazine).
More work is required to increase the cohort and to investigate the
reasons for non-adherence.
P.14.8
DO ULCERATIVE COLITIS PATIENTS TREATED WITH
CORTICOSTEROIDS AT DIAGNOSIS REALLY HAVE A MORE
AGGRESSIVE DISEASE COURSE?
Bertani L.*
1
, De Bortoli N.
1
, Mumolo M.G.
2
, Cosci T.
1
, Laino G.
1
,
Ceccarelli L.
3
, Ricchiuti A.
2
, Bellini M.
2
, Marchi S.
1
, Costa F.
2
1
University of Pisa, Pisa, Italy,
2
Az. Ospedaliero-Universitaria Pisana
- UO Gastroenterologia Univ., Pisa, Italy,
3
ASL1 Massa Carrara - SSD
Endoscopia Digestiva, Carrara, Italy
Background and aim:
Ulcerative colitis (UC) is a chronic relapsing
disease usually treated with mesalamine. In non-responders and in
the more severe cases, corticosteroids (CS) are needed. The need for
CS therapy at diagnosis is generally considered as a poor prognostic
factor. The aim of our study was to assess whether patients treated
with CS at diagnosis have more clinical relapses and/or disease
progression in a 5-year follow up.
Material and methods:
We retrospectively evaluated consecutive
patients who had received diagnosis of UC from 1990 to 2010.
According to NICE Classification, UC was classified as proctitis (P),
proctosigmoiditis (PS), left-side colitis (LC) or extensive colitis (EC).
Relapse was defined as a worsening of symptoms requiring an
increase of medical treatment. Patients were divided in 4 groups
according to the number of relapses in 5 years: Group A (0), Group B
(1-2), Group C (3-4) and Group D (5 or more). Moreover, to evaluate
disease progression, the sub-population of P, PS, LC at diagnosis was
investigated. Progression of disease was defined as the proximal
extension of mucosal involvement.
Statistical analysis was performed by Fisher Exact Test.
Results:
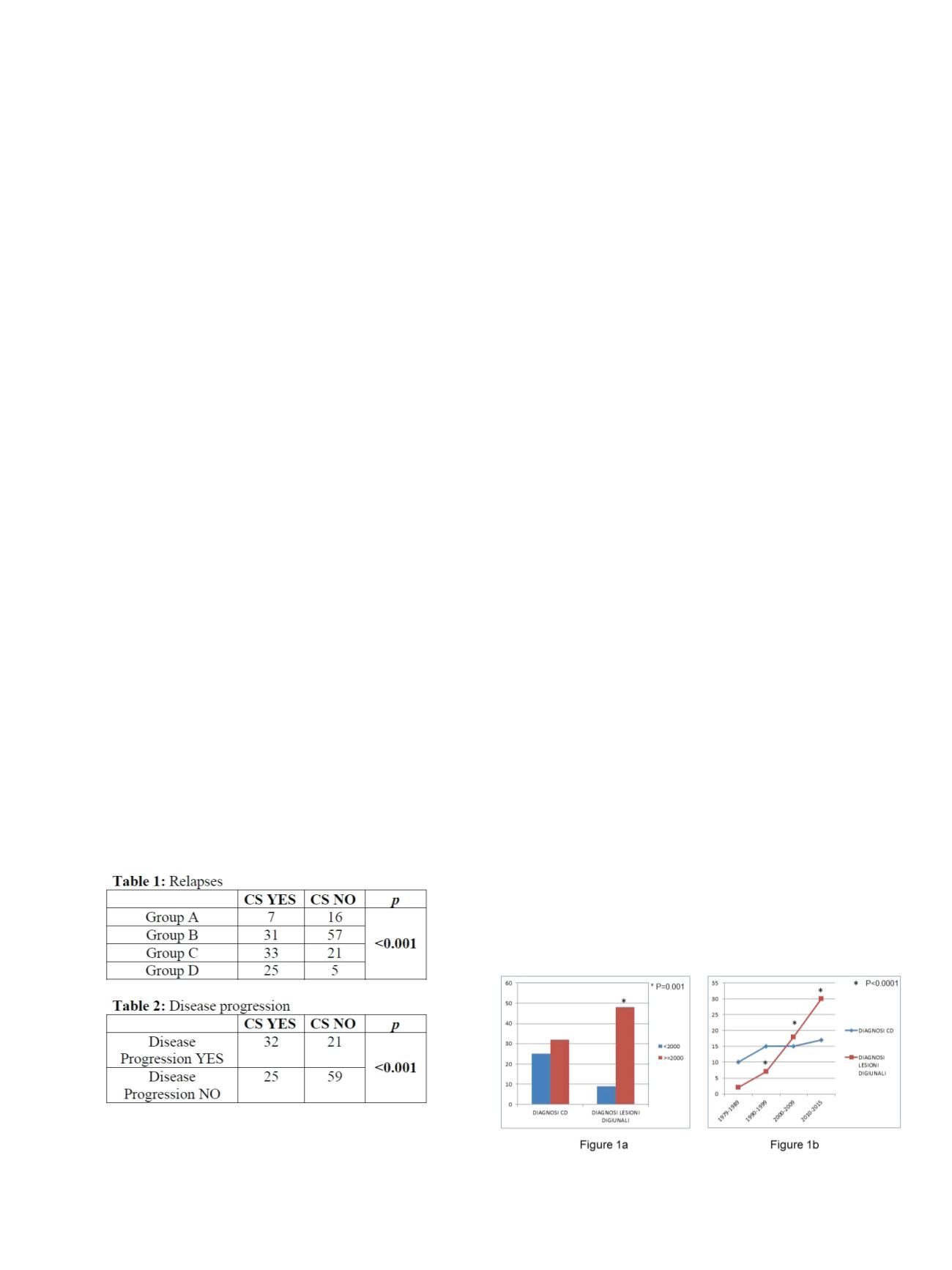
We recruited 195 UC patients (115 M), 96 (49%) treated
with CS at diagnosis. In 5 years, 25/96 (26%) patients had more than
5 relapses with a significant difference if compared to CS-untreated
patients at diagnosis (p<0.001). Results are shown in Table 1.
Out of 137 patients without EC at diagnosis, 53 (38%) showed disease
progression (19 P, 22 PS, 12 LC), of whom 32 (60%) were treated with
CS at diagnosis, in comparison with 21 (40%) treated only with
mesamine (p<0.001). Results are shown in Table 2.
Conclusions:
Our results showed that the use of CS at diagnosis
is strongly correlated with a higher number of relapses during a
long-lasting follow up. Moreover, we demonstrate the correlation
between the need of CS at diagnosis and the proximal extension of
mucosal involvement. These data provides evidence that the need of
CS at diagnosis is associated with a worse clinical outcome.
P.14.9
JEJUNAL CROHN’S DISEASE: CHARACTERISTICS, OUTCOME, NEED
OF SURGERY AND IMMUNOMODULATORS IN A RETROSPECTIVE
SINGLE-CENTER STUDY
Ruffa A.*, Angelucci E., Petruzziello C., Rossi A., Onali S., Sica G.,
Calabrese E., Lolli E., Pallone F., Biancone L.
University of “Tor Vergata”, Rome, Rome, Italy
Background and aim:
The natural history of Crohn’s Disease (CD)
involving the jeunum is undefined. In a retrospective, single-center
study, we aimed to characterize clinical characteristics and outcome
of all patients (pts.) with jejunal CD referring at our tertiary IBD
center. Whether the frequency of jejunal lesions in CD is increased
during the last years was also investigated.
Material and methods:
Clinical records of all CD pts. with complete
data, followed up from 2000-2015 (for ≥1yr) were retrospectively
reviewed. All clinical characteristics were prospectively
recorded, including: gender, age and CD behavior (at diagnosis,
current): B1=non-stricturing non-penetrating; B2= stricturing;
B3=penetrating; CD duration (yrs), CD-site (ileum, I:L1; colon, C:
L2; I+C: L3; jejunum+ I with/without C), surgery (Y/N/,≥1), familial
IBD, smoke (Y/N/ex), perianal (PA), appendectomy, comorbidities,
EIM, cancer, steroid-(CS) dependence (Y/N), immunosuppressors
(IS; AZA/6MP/ MTX), biologics (IFX, ADA). Statistical analysis: Data
expressed as median (range), Fisher exact, Chi square tests
Results:
From 2000 to 2015, 57 pts. with jejunal CD were identified
(23 [40.3%] M;34[59.7%] F; age 44 [17-71]; age at diagnosis of CD (27
[12-66] CD duration 12 yrs [1-36]). Lesions at diagnosis of CD
involved: jejunum+I: n=34; jejunum+C n=3; I with/without C: n=20).
Current lesions involed: jejunum+I: n=41; jejunum+C: n=6; I with/
without C, no jejunum n=10. Overall, 42/57 (73.7%) pts required any
intestinal resection and 21/57 (36.8%) jejunal surgery. Behaviour in
jejunal CD was: B1 n=13; B2=36; B3=8, being B2 correlated with the
need of any intestinal surgery (p=0.016 and p=0.023 for 0 vs≥1 and ≤
vs ≥1 surgery), but not of jejunal surgery (p=0.10). Perianal CD was
observed in 18 (31.6%) pts, being correlated with the need of any
intestinal surgery (p=0.025), but not of jejunal surgery (p=0.71),
familial IBD (p=0.07), smoke (p=0.97). Age at diagnosis of CD was
correlated with IS use (p=0.0018), while the relation between IS and
CD behavior was at limit of significance (p=0.055). The diagnosis of
jejunal lesions (but not of CD) significantly increased during the
follow up (1979-89; 1990-9; 2000-2009; 2010-5; p<0.0001) (Fig.1a)
being significantly more frequent after vs before 2000s (p=0.001)
(Fig.1b). Jejeunal CD was correlated with the need of surgery
(p=0.0016 surgery ≤vs >1; p=0.022 surgery 0 vs ≥1). Therapies: CS in
50/57 (87.7%) (B1 n=12; B2 n=31;B3 n=7), IS in 24/57 pts. (42%) (B1
n=2; B2 n=17; B3 n=5), anti-TNFs in 17/54 (29.8%) jejunal CD pts. (B1
n=4; B2 n=11; B3 n=2).
Conclusions:
In a cohort of CD pts., the diagnosis jejunal lesions
(but not of CD) significantly increased during the last decades. The


















