
e196
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
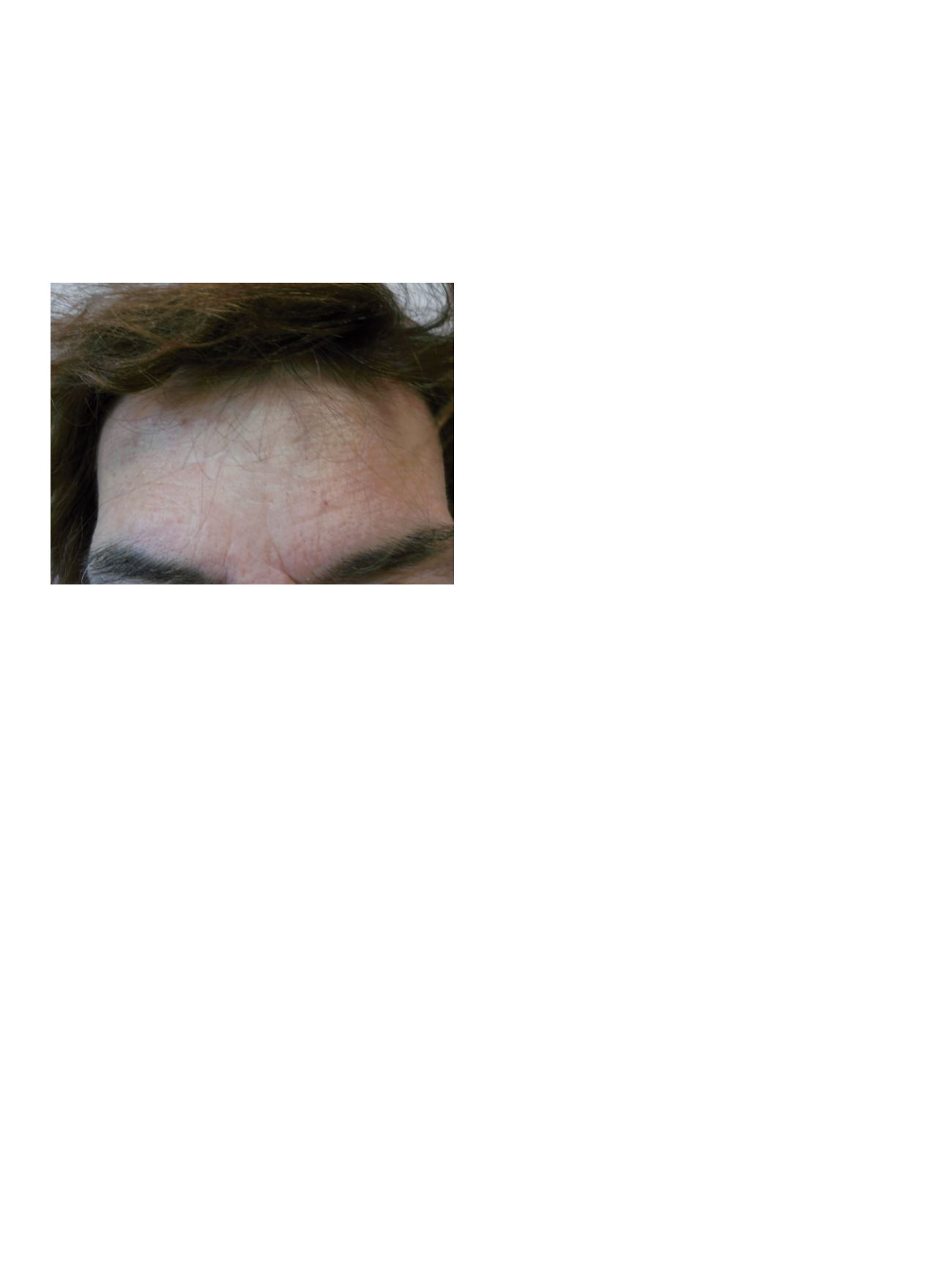
showed focal cronic follicular dermatitis with non caseating
granulomas; periodic PAS and ZiehlNielsen and Gram stains reaction
were negative. A diagnosis of MCD was made, although the patient
refused colonoscopy, we decided to treat with IFX.
Results:
IFX (5 mg/kg of body weight) was administered at weeks 0
(first dose 09/2010), 2 and 6 and every 8 weeks, after 3th infusion
we observed marked improvment and after 5th infusion complete
resolution of the lesions. The treatment was continued to 18 months
and 3.2012 was interrupted. A follow-up was started, we revised the
patient every 12 weeks and after 42 months non relapse was
observed.
Conclusions:
MCD is a rare cutaneous manifestation of active CD
of variable clinical appaearance remote from bowel. Diagnosis
is difficult and must be differentated from infectious and non
infectious skin’s disease; skin biopsy should be performed to
assess characteristic granulomas of CD and rule out infection or
other etiologies; the treatment is not standardized. Our experience
suggest that: 1) MCD can be not related to active intestinal CD; 2)
IFX can be a effective and well tolerated treatment; 3) efficacy of IFX
is very fast; 4) the effect of IFX remains long after discontinuation
of therapy.
P.14.6
PREVALENCE AND CLINICAL SIGNIFICANCE OF
HYPERGAMMAGLOBULINEMIA IN INFLAMMATORY BOWEL
DISEASE PATIENTS: A RETROSPECTIVE CROSS-SECTIONAL STUDY
Menasci F.*, Pagnini C., Desideri F., Sanna A., Delle Fave G.
Sapienza University, Sant’Andrea Hospital, Rome, Italy
Background and aim:
Hypergammaglobulinemia (HGG) is an
alteration commonly described in patients with autoimmune,
infective or inflammatory disorders where an increment of
antibodies production is observed. No data are available for the
prevalence and clinical significance of HGG in inflammatory bowel
disease (IBD) patients. Aim of the present study was to evaluate
the prevalence and clinical significance of HGG in IBD patients in a
retrospective cross-sectional study.
Material and methods:
We included IBD patients referred at S.
Andrea Hospital in Rome, Italy, in outpatient visit, between January
2013 and December 2014. Inclusion criteria were: firm diagnosis of
IBD [ulcerative colitis (UC) or Crohn’s disease (CD)], and complete
records of clinical [age, sex, localization, comorbidities, extra-
intestinal manifestations (articular, dermatologic or ocular IBD-
related diseases), disease activity, presence of flare at 1 year of follow-
up) and biochemical [hemoglobin, C reactive protein, presence
of HGG (defined as polyclonal increment of the gammaglobulins
level above the normal lab-reported value)] parameters. Exclusion
criteria were: uncertain diagnosis, presence of monoclonal HGG,
hematologic or autoimmune disorders. From a total of 388 IBD
patients, 81 patients were excluded (uncertain diagnosis=12, lack
of data=64, monoclonal HGG=3, multiple myeloma=1, autoimmune
thrombocytopenia=1). 307 patients were included (UC=212, CD=95).
Prevalence of HGG was calculated. Clinical and biochemical features
in patients with and without HGG were compared by t-test and chi-
squared test for parametric and non parametric data, respectively.
Multivariate analysis was performed with presence of HGG set as
independent variable. Odd Ratio (OR) and 95% Confidence Interval
(CI) were calculated.
Results:
HGG was found in 46/307 (15%) of IBD patients [CD: 11/84
(13%), UC: 35/177 (20%)]. IBD patients with HGG had significant
higher prevalence of UC (76% vs. 68%, p=0.05) and extra-intestinal
manifestations (28% vs. 14%, p<0.05). At the multivariate analysis,
UC (p<0.05) and extra-intestinal manifestations (p<0.005) were
independently associated with presence of HGG. UC patients with
HGG had significant higher association with presence of extra-
intestinal manifestation than UC patients without HGG (OR 4.5,
95%CI 1.6 to 12.1, p=0.0032), while CD patients with HGG did not
displayed significant difference (OR 2.3, 95%CI 0.7 to 8.5, p=0.19).
Conclusions:
In the present retrospective study, HGG was quite
frequent in IBD patients, and it was associated with higher
prevalence of extra-intestinal manifestation in UC patients.
P.14.7
DRUG ADHERENCE IN IBD PATIENTS
Bucci C.*
1
, Cersosimo G.
2
, Tammaro S.
3
, Iovino P.
1
, Ciacci C.
1
1
Gastroenterologia, University of Salerno, Salerno, Italy,
2
Sociologia
della Salute e della malattia, Università di Salerno, Salerno, Italy,
3
Unità di endoscopia digestiva, P.O. Fucito, Mercato San Severino, Italy
Background and aim:
Therapeutic adherence to multiple drugs has
become one of the major issues in the management of inflammatory
bowel disease (IBD), especially in remission periods. A recent
review showed that non-adherence rates ranged from 7 to 72%,
and a scarce adherence has been associated with frequent relapses,
more complications and increased social costs. Aim of the present
study was to investigate the rate of non-adherence among our IBD
patients.
Material and methods:
Patients were recruited at a IBD referral
centre of the University Hospital in Salerno (Italy). All patients with
a scheduled office visit were asked to fill in a self-administered and
anonymous questionnaire available online on a specific website.
The questionnaire explored in the long-, middle- and short-
period (months, weeks and days, respectively) the adherence to
the 4 major class of drugs used as long term therapy (mesalazine,
immunosoppressors (IMM), steroids and biologic). Also, the
presence of confounders (travels, harassment of taking drugs in
social contests, being worried of adverse events) and the severity of
the disease were considered.
Results:
Complete data are available on 37 IBD patients (63,4% male,
age 21-30 years, 48% Crohn’s disease, 52% RCU). 62% were in clinical
remission, 80% were on mesalazine, 32% on mesalazine plus an IMM
drug, and 21% on mesalazine plus a biologic drug. About half of the
patients (46%) were totally compliant to the prescribed therapy,
while mesalazina was the most frequently forgotten drug among
non-adherent patients. The patients showed a good adherence to
IMMs, steroids and biologics in the long, middle and short term
period. When adherence was evaluated according to disease activity,
12 (30%) of the patients admitted to forget mesalazine when in
clinical remission, 7% forgot IMMs and 10% forgot to inject biologics
or to show up at clinical appointment for anti-TNF infusion. When
outside home, patients tended to forget mesalazine (10%), but none


















