
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e201
mean size was 9 mm (range 5-12 mm). The invasion depth was
limited to the submucosal layer. R1 resection was present in 2 cases
(one after EMR and one after HESD). All lesions were G1-G2 tumors
with <1-2 mitosis per high power field. Ki67 proliferation index
was 2-4% in 4 tumors and 16% in one. One immediate perforation
occurred and was treated conservatively. During the mean follow-up
period of 17 months (range 6-31) no local recurrence was observed.
A liver metastasis was diagnosed one year after ER in one patient.
Conclusions:
Duodenal ER has a higher incidence of complications
than in other sites of gastrointestinal tract because of the thickness
duodenalwall. Despite en-bloc resectionwas performed, R0 resection
was present in only 60% of cases. We suppose that such result is due
to the paucity and laxity of submucosal duodenal tissue, which is
destroyed during ER. In fact, because of the narrow duodenal lumen,
to avoid excessive burning of peritumoral submucosal duodenal
tissue may be technically difficult. To support this hypothesis we did
not observe any local recurrence at follow-up UGIE. Our experience,
although limited and retrospective, confirms the safety and efficacy
of ER for the treatment of dNETs limited to the submucosal layers.
However, additional studies with longer follow up are needed.
P.15.2
NEO-ENDOSCOPIC CUL DE SAC OTSC MADE IN DELAYED
SURGICAL COMPLICATION
Staiano T.*
3
, Martinotti M.
1
, Rispo A.
2
, Buffoli F.
4
1
S.C. Chirurgia Generale A.O. Istituti Ospitalieri di Cremona, Cremona,
Italy,
2
DAI Gastroenterologia, Endocrinologia, Chirurgia A.O.U. Federico
II, Napoli, Italy,
3
S.C. Endoscopia Diagnostica e Chirurgica Endoscopica
Fondazione IRCCS Istituto Nazionale dei Tumori, Milano, Italy,
4
S.C.
Endoscopia Digestiva e Gastroenterologia A.O. Istituti Ospitalieri di
Cremona, Cremona, Italy
Background and aim:
Anastomotic leakage, the most feared
complication of colorectal surgery, is associated with increased
morbidity and mortality, prolonged hospital stay, and additional
health-care costs. Its reported prevalence varies widely from 1 to
39%, but clinically relevant leaks probably occur in 3–6% of cases,
depending on the definition and the type of resection. Where
indicated, operative endoscopy to achieve wound healing may be a
viable alternative, allowing minimally invasive treatment. We report
a case of successful endoscopic closure of chronic double cul de sac
fistulas modifing OTSC application and deployement.
Material and methods:
A 67-year-old man underwent left
hemicolectomy for sigmoid colon cancer. A colocolonic end-to-
side anastomosis was performed. Five months later the patient was
admitted to the intensive care unit because of worsening clinical
status. An anastomotic dehiscence was diagnosed by use of a CT scan
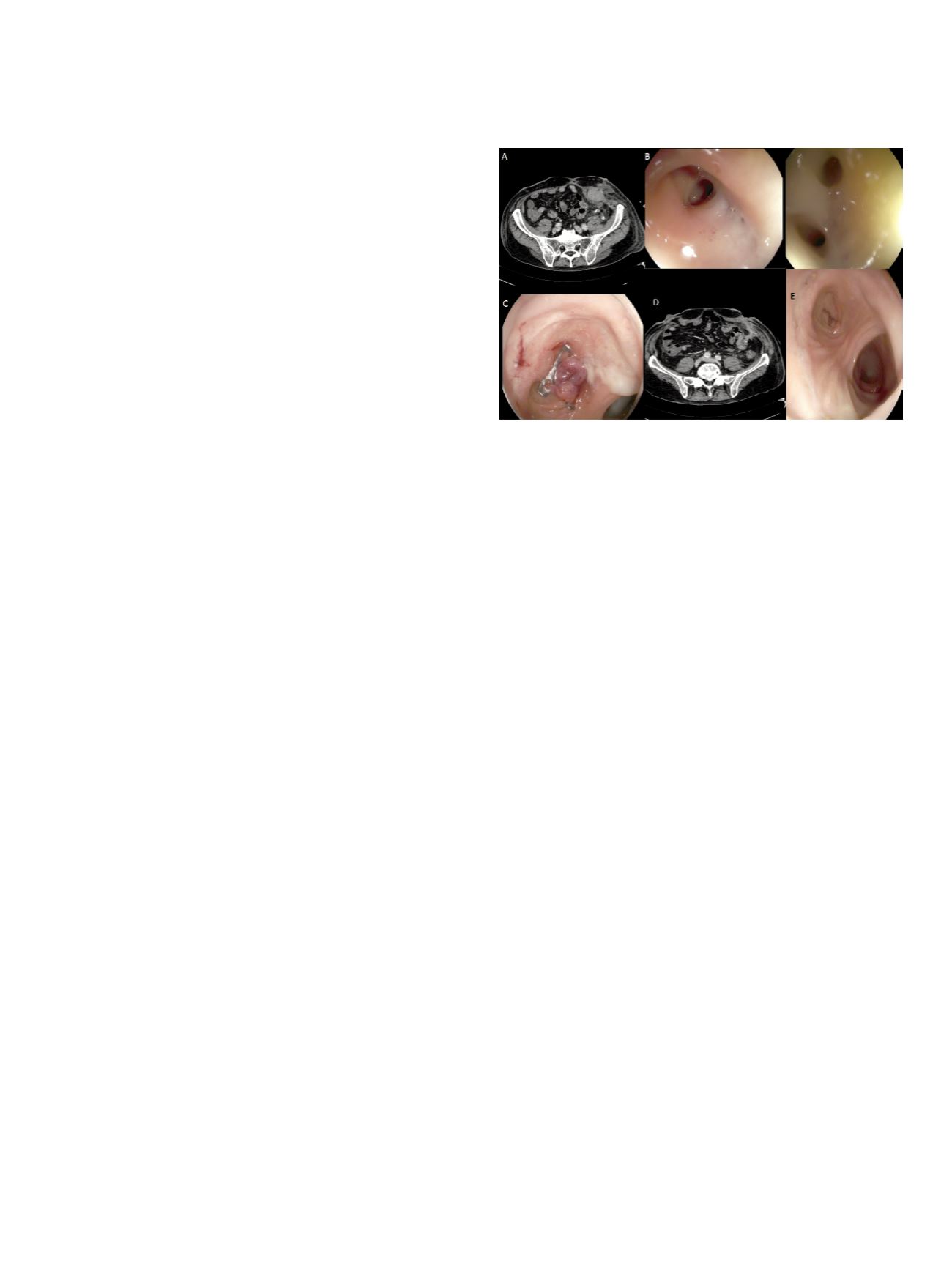
Fig 1 A). Air was also present in the retroperitoneum. Endoscopy was
immediately performed, and two areas of anastomotic dehiscence
of approximately 5 and 10 mm of colocutaneous fistula occurred
in the cul de sac (B). The cap was applied against the fistula, and
aspiration was performed to remove a large amount of collected
fluid and debris outside the colon. The anchor probe was intro-
duced through the fistula and the grasped tissue firmly pulled
inside the cap. Continuous suction was applied to assist traction of
the anchor probe. It was impossible to correctly deploy the OTSC
due to insufficient grasping and suction caused by fibrosis, scarred
and hardened postsurgical tissues at the edges of the lesion. Such, to
allows to capture a large amount of soft tissue above the leakage, we
positioning the device at medial tract of the cul de sac and without
using any grasper. Healthy mucosa were fully pulled and suctioned
into the cap, then the clip was deployed (C).
Results:
The patient was allowed to have a full diet 24 hours later,
after a Gastrografin enema confirmed sealing. The patient was
discharged from the hospital 1 week later. CT scan performed 1
month after hospital discharge confirmed that the leakage was
sealed (D). Endoscopy confirmed a new cul de sac, with healthy
mucosa without OTSC (E).
Conclusions:
Endoscopic OTSC (Over-the-Scope Clip (OTSC®;
Tübingen, Germany) application is an especially attractive option
for the treatment of small leakages and fistulas. It allows the
closing of defects by grasping much larger amounts of tissue with
a high compression force. Some studies reported a lower efficacy
for treatment of chronic fistulas. In a recent case series including 9
patients, the overall success rate of OTSC application was 55%; it was
impossible to correctly deploy the OTSC due to insufficient grasping
of the tissue caused by fibrosis at the edges of the lesion. In our case,
we overcome these limitation aspirating soft and health mucosa
above the scarred and fibrotic tissue, creating a new endoscopic cul
de sac.
P.15.3
INCREASED PERFORMANCE OF AN UPDATED ROCKALL SCORE IN
ACUTE NON VARICEAL UPPER GASTRO INTESTINAL BLEEDING: A
PROSPECTIVE MULTICENTRE ITALIAN STUDY
Marmo R.*, Soncini M., Cipolletta L., Parente F., Paterlini A.,
Bennato R., Cipolletta F., Amitrano L., Bargiggia S., Cesaro P.,
Bizzotto A., Dell’Era A., Germanà B., Cavallaro L.G., Riccioni M.E.,
Marmo C., Tortora A., Segato S., Parravicini M., Purita L.,
Chirico A., Spinzi G., Imperiali G., Merighi A., Boarino V., Bresci G.,
Metrangolo S., Bucci C., Baldassarre G., Franceschi M., Nucci A.,
De Nigris F., Masci E., Marin R., Antoniazzi S., Ferraris L., Repici A.,
Andreloni A., Bianco M.A., De Matthaeis M., Lauri A., De Fanis C.,
Borgheresi P., De Stefano S., Lamanda R., Furio L., Russo A.,
Maringhini A., Politi F., Di Giorgio P., Pumpo R., Martorano M.,
Triossi O., Coccia G., Montalbano L.M., Zagari R.M., Buscarini E.,
Conte D., D’Amico G., Di Giulio E., Balzano A., Gasparini P.,
Rotondano G., De Franchis R.
Gruppo Italiano Studio Emorragia Digestiva,, Rome, Italy
Background and aim:
Patients with acute non-variceal upper
gastro intestinal bleeding (ANV-UGIB) have a wide range of clinical
severity, ranging from patients needing of diagnostic procedures
to patients at death risk. Triaging and differentiating patients in
correct classes of risk could impact on clinical outcomes and on
resource saving. The Rockall score is a widely used and validated
score addressing these issues on hospital admission. In the last
years, factors other than those included in the Rockall score were
studied. Our aim was to evaluate the prognostic value of an updated
Rockall score compared with the traditional one.
Material and methods:
Data on patients admitted for ANV-UGIB
were collected from January 2014 to September 2015. Primary


















