
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e119
V.01 Video 1
V.01.1
GASTROSCOPIC REMOVAL OF A MIGRATED ADJUSTABLE GASTRIC
BAND: A CASE REPORT
Balzarini M.*
1
, Colombo A.
2
, Calcara C.
1
, Broglia L.
1
, Alonzo A.
2
1
Gastroenterologia Ospedale SS Trinità ASL Novara, Borgomanero,
Italy,
2
Chirurgia Ospedale SS Trinità ASL Novara, Borgomanero, Italy
Background and aim:
Laparoscopic gastric banding is a popular
method for treating morbid obesity. Intragastric band migration
in an unusual but major complication of gastric banding. When
migration occurs, band removal is mandatory to prevent intra
abdominal infection, gastrointestinal obstruction or life threatening
hemorrage and the treatment is usually reoperation.
Material andmethods:
A 43 years old female patient, with suspected
band migration caused by vomit, underwent an upper endoscopy
showing a partial transgastric migration of the laparoscopic
adjustable silicone gastric band (LASGB). With the patient under
general anesthesia, through a cutaneous exploration at the port-
site, the silicone connecting tube was resected and the injection port
extracted. The band was then retrieved endoscopically.
Results:
After insertion of the gastroscope and insufflation of the
stomach with CO2 the migrated band was identified. A standard
ERCP guidewire was introduced into the working port of the
endoscope and passed between the partially migrated LASB and the
stomach wall and picked up at the other side of the LASB, creating a
noose around the band. Both end of the guidewire were externalized
through the mouth. The metal spiral sheath of a mechanical ERCP
lithotriptor was passed over both ends of the wire. The metal tube
(containing the guidewire looped around the intragastric band)
was passed through the esophagus to the stomach. By twisting
the handle of the gastric lithotriptor the band was cut under
direct vision. The band was than retrived endoscopically by using
a polypectomy snare. Finally the gastroscope was again introduced
to check visually the full integrity of the gastric wall. No other
complementary postoperative examination was performed and the
patient was discharged the day after. The patient was reexamined
gastroscopically one month after the removal of the LASB to confirm
adequate closure of the migration defect
Conclusions:
In this case report we show that a band penetrating
the gastric wall can be treated endoscopically using standard
equipment. It seems that this technique is simpler than reoperation
and is beneficial even when the intraluminal migration is partial.
The use of standard endoscopic equipment makes the procedure
feasible in almost all the endoscopic units.
V.01.2
PER-ORAL ENDOSCOPIC MYOTOMY (POEM) WITH A NEW
THERAPEUTIC LASER SYSTEM: FIRST STUDY IN AN EX VIVO
ANIMAL MODEL (WITH VIDEO)
Tontini G.E.*
1
, Neumann H.
2
, Carmignani L.
3
, Bruni B.
4
, Soriani P.
1
,
Pastorelli L.
1
, Fagnani F.
5
, Clemente C.
4
, Bottani M.
1
, Vecchi M.
1
1
Gastroenterology & Digestive Endoscopy Unit, IRCCS Policlinico San
Donato, San Donato Milanese, Milano, Italy,
2
Department of Medicine
I, University of Erlangen-Nuremberg, Erlangen, Italy,
3
Academic
Urology Department, IRCCS Policlinico San Donato, San Donato
Milanese, Milano, Italy,
4
Pathology and Citodiagnostic Unit, IRCCS
Policlinico San Donato, San Donato Milanese, Milano, Italy,
5
Surgical
Division, Quanta System SpA, Varese, Italy
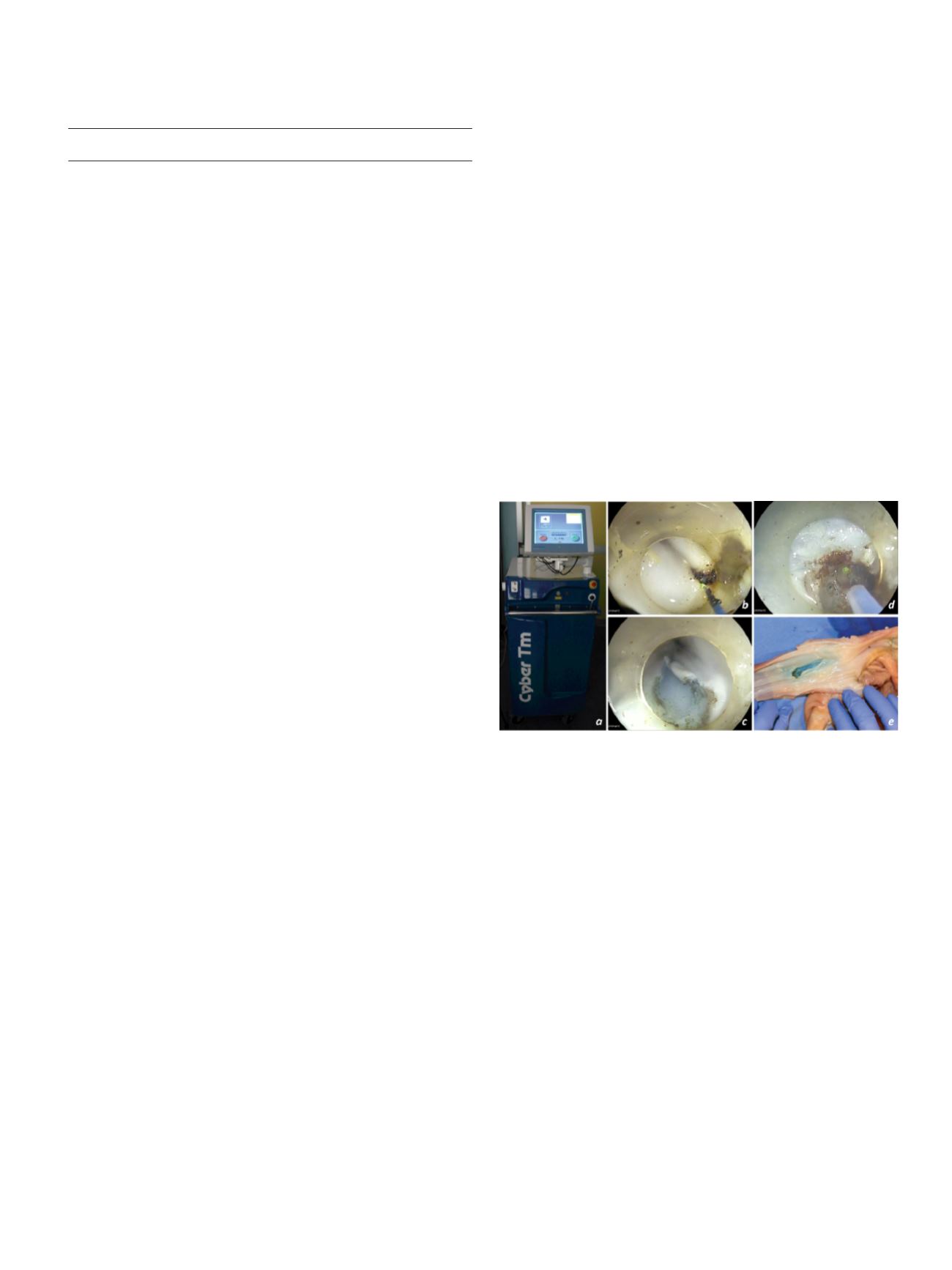
Background and aim:
Several therapeutic laser systems are
established for surgical and endourlogical interventions [1-2].
Most recently, a new therapeutic laser system with a wavelength of
2μm has been developed to provide constant speed of cutting and
vaporization (i.e. “vaporesection”) with a precise control on depth
and lateral tissue penetration to avoid inadvertent injury (fig. a).
To date, no study has assessed the efficacy of the new device for
gastrointestinal endoscopy. We conducted the first pilot study to
test the feasibility of the newly introduced Thulium laser system
(Cyber TM®, Quanta System, Varese, Italy) for POEM by using an
established experimental setting (EASIE model).
Material and methods:
The POEM procedure was performed
following a standard technique. All steps were performed just by
using the new Laser system and video-recorded. Subsequent to
the endoscopic procedure, specimens were evaluated by an expert
pathologist.
Results:
A complete POEM by using the Thulium laser took approxi
mately 20 minutes. No perforation to the luminal side (i.e. mucosal)
occurred (fig. b-e). For laser power settings the most effective choice
was 25-35 watts for mucosal excision and 15-25 watts for
submucosal and muscular excision. Histopathology confirmed a
clean and safe cutting of the different layers.
Conclusions:
This is the first study of the newly introduced Thulium
laser system showing the safety and efficacy of the new device for
performing POEM procedures. These promising results should now
be confirmed in additional in vivo studies.
References:
1. Rieken M & Bachmann. Nat Rev Urol 2014.
2. Carmignani L, et al. Asian J Androl 2015.
V.01.3
ENDOSCOPIC BANDING FOR ABLATION OF DUODENAL FLAT
LESIONS IN HIGH RISK PATIENTS
Parzanese I.*, Rosa R., Tenca A., Conte D., Penagini R., Cantù P.
Gastroenterology and Endoscopy Unit, Fondazione IRCCS Cà Granda,
Ospedale Maggiore Policlinico, Department of Pathophysiology and
Transplantation Università degli Studi di Milano, Milan – Italy, Milan,
Italy
Background and aim:
Non-ampullary duodenal flat lesions are
usually managed with endoscopic mucosal resection (EMR) but a
high rate of perforation and bleeding has been reported.
Aim was to evaluate the safety and effectiveness of endoscopic
banding (EB) as an alternative technique to EMR for ablation of
duodenal flat polyps in patients at high risk for complications.
Material and methods:
FromMay 2013 to May 2015, we treated five
patients (3 M, age 34-70) with high (#2) or low (#3) grade dysplastic
adenomatous flat polyps (8-15 mm) of the duodenum. In four cases
Video


















