
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e123
V.01.11
IN VIVO ASSESSMENT OF TUMOR ANGIOGENESIS IN COLORECTAL
CANCER: ROLE OF CONFOCAL LASER ENDOMICROSCOPY
De Palma G.D., Esposito D.*, Maione F., Luglio G., Siciliano S.,
Gennarelli N., Cassese G., Campione S., D’Armiento F.P., Bucci L.
AOU Policlinico Federico II, Naples, Italy
Background and aim:
Tumor neoangiogenesis is a key factor for
tumor progression and metastatic spread. The possibility to assess
tumor angiogenesis might provide prognostic information. Aim of
the study was to establish the role of probe-based Confocal Laser
Endomicroscopy (p-CLE) in the identification of vascular architecture
and specific morphological patterns in normal colorectal mucosa
and malignant lesions, during routine endoscopy.
Materialandmethods:
Fourteenconsecutivepatientswithcolorectal
cancer were included. The following features were identified and
then compared between normal and neoplastic mucosa on p-CLE
images: vessel shape (straight vs irregular); vessel diameter; the
“branching patterns”; vessel permeability (fluorescein leakage)
and blood flow (normal vs defective flux). Immunohistochemistry
was used to confirm the presence and to study the morphology
of vascular structures (CD-34 staining) and “neo-vessels” (WT-1
staining) on tumor and normal mucosa sections.
Results:
Tumor vessels appeared as irregular, ectatic and with a
highly variable caliber and branching patterns on p-CLE images.
Mean diameter of tumor vessels was significantly larger when
compared with normal mucosa (WMD, 3.38, 95% CI 2.65, 4.11,
p=0.01). Similarly, “vessel branching” (OR, 2.74, 95% CI 1.23, 6.14,
p=0.01), fluorescent dye “extravasation” (OR, 3.46, 95% CI 1.39, 8.57,
p=0.01) were significantly more frequent in colorectal cancer than
in normal colorectal mucosa. Immunohistochemistry corroborated
p-CLE findings, showing higher vascularity in tumor sections due to
neo-formed vessels, presenting irregular patterns as shown at p-CLE
images.
Conclusions:
P-CLE provides a non-invasive characterization
of the microvascular architecture of colonic mucosa. Different
morphological patterns have been described, discriminating from
normal and malignant microvascular networks in colorectal mucosa.
V.01.12
OVER-THE-SCOPE CLIP-ASSISTED ENDOSCOPIC FULL THICKNESS
RESECTION AFTER INCOMPLETE RESECTION OF RECTAL
ADENOCARCINOMA: CASE AND VIDEO REPORT
Soriani P.*
1
, Tontini G.E.
1
, Pastorelli L.
2
, De Nucci G.
3
, Steffano G.B.
4
,
Di Fratta E.
4
, Vecchi M.
1
, Lagoussis P.
4
1
Gastroenterology & Digestive Endoscopy Unit, IRCCS Policlinico San
Donato, San Donato Milanese, Milano, Italy,
2
Italy,
3
Gastroenterology
& Digestive Endoscopy Unit, AO Salvini, Garbagnate Milanese, Italy,
Italy,
4
Division of General Surgery I, IRCCS Policlinico San Donato, San
Donato Milanese, Milano, Italy
Background and aim:
The endoscopic resection is a valuable
therapeutic option for early colorectal cancer (CRC), especially in
high-risk surgical patients [1]. A novel endoscopic full-thickness
resection device (FTRD; Ovesco Endoscopy, Tübingen, Germany) has
been recently introduced to achieve complete resection of early CRC
during ongoing endoscopy [2].
Material and methods:
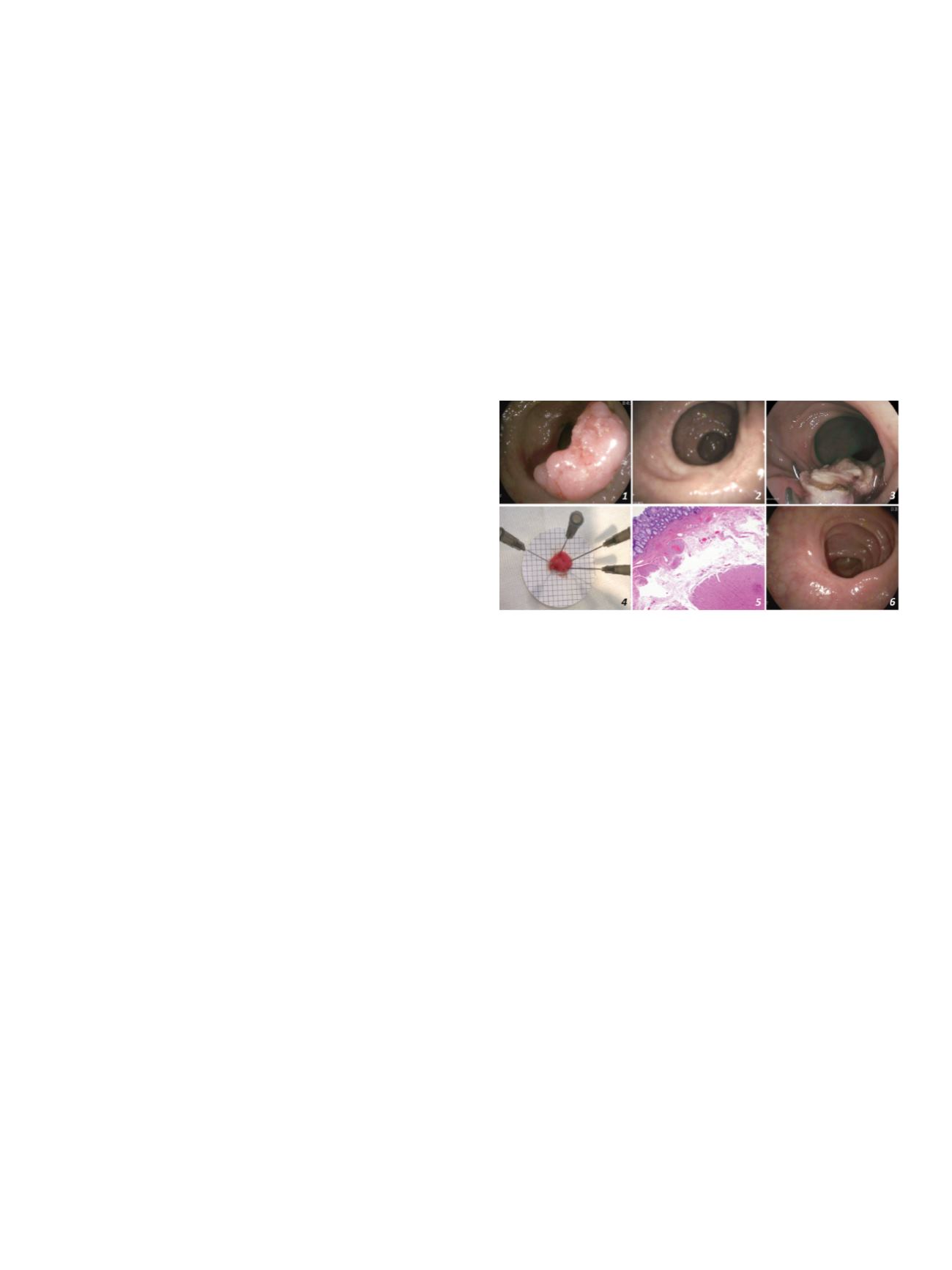
Here, we report the case of a 78-year-old
man with a history of coronary disorders and recent pulmonary
embolism who underwent colonoscopy for hematochezia. A 3 cm,
non-pedunculated colorectal polyp with adenomatous pit pattern
(Kudo IV) was observed 5 cm above the dentate line (fig.1). An en bloc
endoscopic mucosal resection was performed. Histology revealed
adenocarcinoma pT1 G2 Sm3, while total body CT scan and rectal
endoscopic ultrasound reveal no lymphatic or metastatic disease.
Based on patient’s comorbidities, we used FTRD to achieve the R0
resection (Video) after antibiotic prophylaxis with intravenous
cefalosporine.
Results:
First, lateral margins of the scarred resection site were
marked with argon plasma coagulation (fig.2). The device was
mounted on the tip of a standard gastroscope and, through a tissue
anchor, the whole scarred lesion was pulled in to the cap and the
OTSC was deployed. The pseudopolyp tissue created by the OTSC
was resected using the pre-loaded snare and standard electrosurgical
setting (VIO® ERBE Elektromedizin GmbH, Tübingen, Germany). The
procedure took about 8 minutes and no bleeding nor perforation
occurred (fig. 3). Patient reintroduced anticoagulant agents and was
discharged in perfect condition the following day. On the full-
thickness 15 mm-large specimen (fig.4), histological analysis
revealed no remnant dysplasia (fig.5), as well as in the biopsy
samples taken from the clear rectal scar 3 months later (Fig 6).
Following endoscopic ultrasound and CT scan confirmed the absence
of lymphatic or metastatic disease and abscess.
Conclusions:
This case is interesting for several reasons. First,
we have performed for the first time a full-thickness endoscopic
resection for early CRC in the distal rectum, where standard surgery
imply considerable risks and aggressive strategies. Secondly, we
evaluated the potential of the novel FTRD in a high-risk patient
with ongoing anticoagulants therapy. In addition, we have shown
in detail the long-term clinical and endoscopic outcomes of this
advanced endoscopic treatment.
References
:
1. Rutter MD, et al. Gut 2015;0:1–27.
2. Schmidt A, et al. Endoscopy 2015;47:719-25.
V.01.13
ENDOSCOPIC LIGATION AND RESECTION OF A LARGE
SYMPTOMATIC SUBEPITHELIAL TUMOR OF THE DUODENUM
Antonini F.*, Belfiori V., De Minicis S., Lo Cascio M., Marraccini B.,
Piergallini S., Rossetti P., Andrenacci E., Macarri G.
Ospedale A.Murri, Fermo, Italy
Background and aim:
Subepithelial tumors (SETs) are frequent
findings during endoscopy. Definitive diagnosis based on endoscopic
biopsies is often not feasible, while endoscopic ultrasonography
(EUS) is good to differentiate the nature of SET and can help guide
decisions about treatment. Surgical resection is the gold standard
for treatment of symptomatic gastrointestinal SETs, however novel
endoscopic procedures represent an alternative to surgery in
selective cases.
Material and methods:
We here report a case of a 55 years-old
woman presented for severe anemia and melena with an history
of nonsteroidal anti-inflammatory drugs use. Upper endoscopy
revealed a peduncolated SET of about 30 mm, ulcerated with
a central bleeding stigmata, located in the second part of the
duodenum. Biopsy of the lesion were inconclusive. EUS revealed


















