
e126
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
V.02.6
ENDOSCOPIC SUBMUCOSAL DISSECTION OF A LARGE PSEUDO-
DEPRESSED SUPERFICIAL NEOPLASM OF THE TERMINAL ILEUM
Iacopini F.*
1
, Grossi C.
1
, Saito Y.
2
, Rigato P.
4
, Gotoda T.
3
1
Endoscopy Unit, Ospedale S. Giuseppe, Albano L., Rome, Italy,
2
endoscopy Division, National Cancer Center Hospital, Tokyo, Japan,
3
GI & Endoscopy Unit, Tokyo University, Tokyo, Japan,
4
pathology Unit,
Ospedale S Giuseppe, Marino, Rome, Italy
Background and aim:
It is recognized that superficial tumors of
the duodenum, jejunum and terminal ileum pose a higher degree
of complexity for endoscopic resection and surgical treatment is
sometimes required in cases of incomplete resection. ESD achieves
significantly higher en bloc and complete (R0) resection than
conventional snare resection but is associated with a higher risk of
adverse events, i.e. perforation.
Material and methods:
We report one very rare case of a large
superficial neoplasm of the terminal ileum treated by endoscopic
submucosal dissection (ESD).
Results:
A 73-year-old woman underwent colonoscopy for
abdominal pain after a previous examination performed 3 years
before.
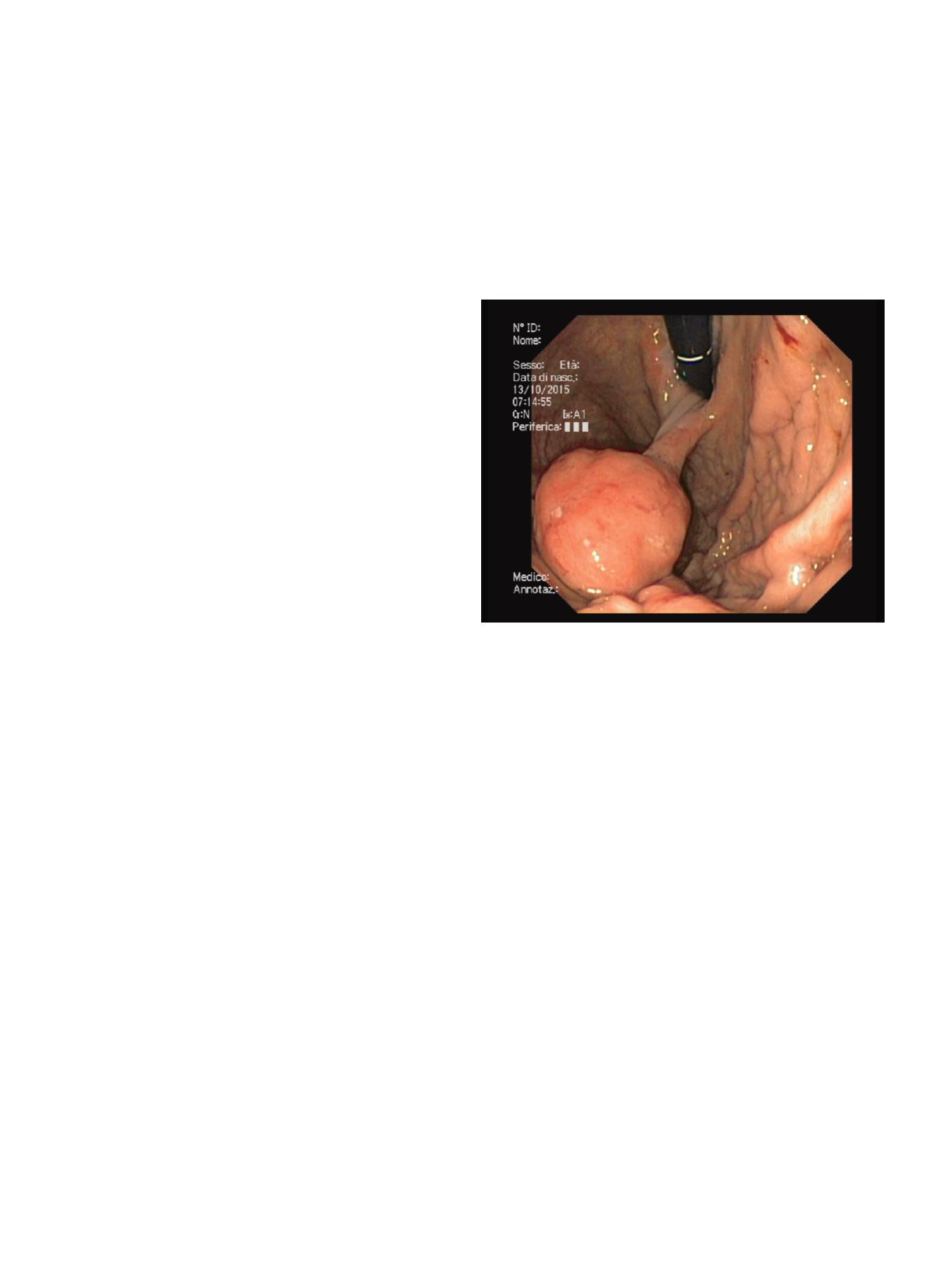
At routine ileoscopy, a large 30x25 mm laterally spreading tumor
non granular with a central pseudodepression (LST-NG PD type) was
incidentially diagnosed. At chromoscopy with indigo carmine and
narrow band imaging, endoscopy showed a Kudo pit pattern type
IIIs ìand a Sano microcapillary pattern type 3A.
The tumor was resected en bloc by ESD with a combination of a
small-caliber-tip transparent hood, insulated and noninsulated
knives, no ncomplication occurred.
Technical difficulties were: indentification of neoplasm borders; the
incision of the mucosal layer due to the presence of villi; the access
into the submucosal layer. A whitish minute (2 mm) submucosal
nodule resulted to be a Peyer’s patch was observed.
Histology of the resected specimen showed an adenoma with low
grade dysplasia with negative lateral and vertical margins.
Conclusions:
ESD in the terminal ileum requires proper anatomical
kwoledges but may achieve successful curative resection with
standard devices without complications.
V.02.7
ENDOSCOPIC RESECTION OF A LARGE PYLORIC GLAND ADENOMA
OF THE CARDIA
Togliani T.*, Mantovani N., Vitetta E., Savioli A., Troiano L., Pilati S.
S.S.D. di Endoscopia Digestiva, Azienda Ospedaliera Carlo Poma,
Mantova, Italy
Background and aim:
Pyloric gland adenomas represent less than
3% of gastric polyps, with a strong predominance in elderly females.
In the stomach the gastric body is the most common location,
although extragastric sites such as duodenum, gallbladder, Wirsung
duct and uterus have been described. They are characterized by
closely packed pyloric gland-type tubules that express MUC6, and
an association with intestinal metaplasia, autoimmune gastritis or
dysplasia is not rare. Anemia, which is the most common clinical
onset, can be due either to blood loss or to vitamin B12 deficiency in
the setting of atrophic gastritis. Given the risk of coexisting cancer,
an endoscopic or surgical resection is advisable.
Material and methods:
A 69-year-old man presented with iron-
deficiency anemia. Colonoscopy was unrevealing. Upper GI
endoscopy showed a 4 cm round peduncolated lesion hanging in
the gastric fundus from the cardia, with some small erosions on
the overlaying mucosa. At EUS the head of the polyp consisted of
a slightly hyperechoic inhomogeneous submucosal mass with
internal anechoic cystic spaces; the superficial mucosal layer was
normal; no Doppler-positive structures were visible in the stalk;
no regional lymph nodes were visible. Afterwards, using a large
working channel gastroscope, we put an endo-loop at the base of
the stalk, we resected the lesion with a snare and we retrieved the
polyp for histology.
Results:
No early complications occurred and the patient was
discharged two hours after the procedure. Histology revealed a 4.5
cm pyloric gland adenoma with no dysplastic alterations; the
superficial epithelium showed a lymphocytic Helicobacter pylori-
positive chronic gastritis. At the time of writing this paper neither
an upper GI endoscopy nor a blood cell count have been repeated
yet.
Conclusions:
This is a case report of a rare large pyloric gland
adenoma; its anatomical location and the male sex of the patient
make the case much more uncommon. A preliminary EUS allowed
to exclude major inner vascular structures before polypectomy; the
endoscopic resection was complete and without complications.
Given the need for an en-bloc removal, for providing the pathologist
an intact polyp, the extraction of a big lesion through the cardia and
the upper esophageal sphincter can represent the main technical
difficulty of the procedure.
V.02.8
EFFECTIVE ENDOSCOPIC HOLMIUM LASER LITHOTRIPSY IN
THE TREATMENT OF A LARGE IMPACTED GALLSTONE IN THE
DUODENUM
Mirante V.G.*, Bertani H., Grande G., Manno M., Caruso A.,
Mangiafico S., Conigliaro R.
U.O.C. Gastroenterology and Digestive Endoscopy Unit, Nuovo
Ospedale Civile Sant’Agostino Estense, Modena, Italy
Background and aim:
Gallstone ileus is caused by the passage
of one or more large gallstones (at least 2.5 cm in size) in the
gastrointestinal tract through a bilio-enteric fistula. It accounts
for 1-4% of all cases of mechanical small bowel obstruction. The
obstructing gallstone usually impacts the terminal ileum, rarely the
duodenum. CT scan usually reveals mechanical bowel obstruction,
pneumobilia and ectopic stone in the intestinal lumen (Ringler’s
triad). Although surgery is considered the gold-standard treatment,
a less invasive endoscopic approach is advisable in high risk patients.
Material and methods:
A 87 years old woman was admitted to
the emergency department complaining of abdominal pain and
vomiting for three days. CT scan showed a large, calcified ring in
the duodenum and aerobilia. An upper endoscopy revealed the


















