
e124
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
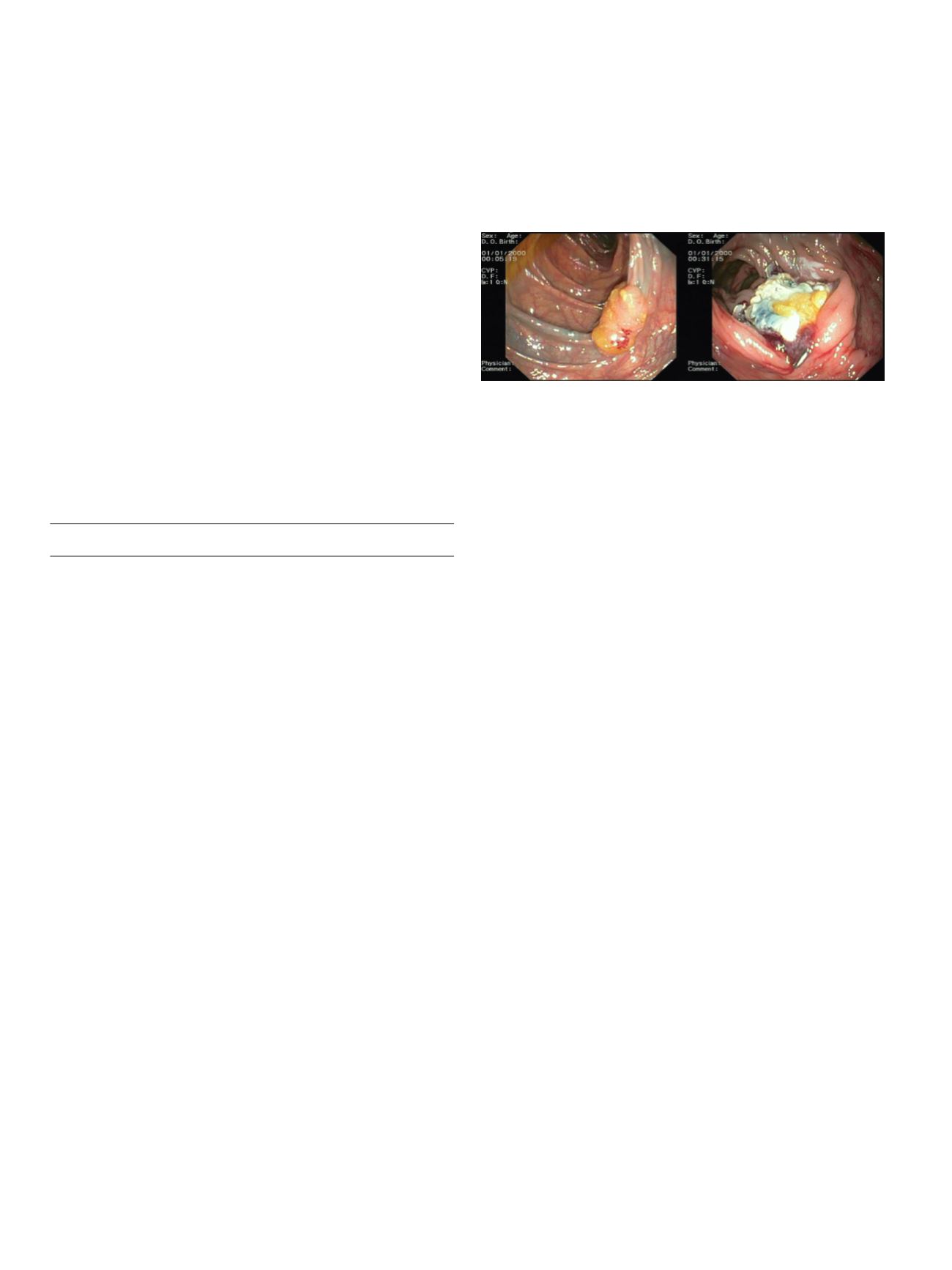
an heterogeneously hypoechoic mass with cystic anechoic spaces,
arising from the third layer. We planned to perform an endoscopic
resection. The excision of the SET was performed by standard oval
electrosurgical snare after placement of a detachable nylon endoloop
to the base of the stalk. Non procedure-related complication
occurred. An endoclip was applied to secure the stalk. The resected
lesion was then placed in a net polyp retriever and extracted back
through the mouth. It was a well-circumscribed mass of 30×20
mm, with an ulcerated surface and yellowish tissue on resection
margin. Histopathologic examination estabilished a diagnosis of
lipoma without atypical cells. After 3 months follow-up, patient was
persistently asymptomatic and an upper endoscopy was performed
without any evidence of lesions.
Results:
Endoscopic resection of large lipomas may be associated
with complications, as the low water content of fat makes it poor
conductor of electrosurgical current. The use of a detachable snare
may reduce the risk of bleeding. EUS in this case has proven to be
essential for determining the original layer of SET and subsequent
treatment.
Conclusions:
Endoloop-assisted endoscopic resection can be one
of the reliable therapeutic options for patients with peduncolated
symptomatic SETs, given its low risk profile and provision for
effective en bloc removal.
V.02 Video 2
V.02.1
4 CASES OF ENDOSCOPIC FULL-THICKNESS RESECTION OF
COLONIC LESIONS USING OVESCO FTRD® SYSTEM: OUR
EXPERIENCE
Ferronato A.*
1
, Franceschi M.
1
, Messina O.
1
, Tomba F.
1
, Sella D.
1
,
Visonà A.
3
, Vanzetto E.
2
, Toffanin R.
4
, Antonelli O.
1
, Biasi M.
1
,
Busellato V.
1
, Calgaro C.
1
, Capillati M.
1
, Baldassarre G.
1
1
UOSVD Endoscopia ULSS 4 Alto Vicentino, Santorso (VI), Italy,
2
Direzione Medica Ospedaliera ULSS 4 Alto Vicentino, Santorso (VI),
Italy,
3
UO Anatomia Patologica e Citodiagnostica ULSS 4 Alto Vicentino,
Santorso (VI), Italy,
4
Direzione Sanitaria ULSS 4 Alto Vicentino, Thiene
(VI), Italy
Background and aim:
OVESCO AG recently proposed a novel
therapeutic tool (FTRD® system) for the resection of adenomas of
the colon and the rectum. It permits an endoscopic full-thickness
resection (eFTR) of lesions, enabling the endoscopist to resect all
layers of suitable lesions including the serosa. We discuss here the
first 4 cases of eFTR performed in our Endoscopic Unit.
Material and methods:
From March 2015 we performed 4 FTRD to
4 patients, 2 men and 2 women, mean age 65 years (range 54-81).
Lesion localization was 1 hepatic flexure, 1 transverse colon, 1 sigma
and 1 rectum. Lesions had different morphological characteristics as
to Paris-Kyoto classification: 0 – IIc, 0 – IIc + IIa, 0 – IIa + IIc and 0 –
Is. Lifting sign was negative in all lesions. 2 lesions were recurrent
polyps after prior polypectomy. Histopathology showed an early
carcinoma and 3 adenomas with high-grade dysplasia. One patient
was not eligible to surgery due to atrial fibrillation, severe ischemic
cardiomyopathy and chronic renal failure.
FTRD® system consists on a 21 mm cap with a clip and a snare,
applied on the tip of a standard endoscope, which is covered with a
sleeve. It slightly reduces visibility and handling of the scope during
the exam. The procedure has 4 steps: marking, grasping inside the
cap, releasing the clip then electrical snare cut of the lesion.
Results:
eFTR was successful in 3 of 4 procedures. In one patient
eFTR failed due the inability to retrieve the complete lesion inside
the cap, therefore she was referred to surgery. Elective surgery
revealed a neoplasm invading the perirectal fat. The other 3 patients
had a complete lesion removal confirmed by histology. All patients
were dismissed after a 3 hours observation period after the
procedure without any symptom. No adverse events were observed
in a minimum 4 months follow-up. Patients with successful eFTR
underwent a control colonoscopy after 2-3 months revealing a good
healing of the resection.
Conclusions:
eFTR with OVESCO FTRD® system is easy to perform
and permits a radical resection of advanced adenomas not resectable
with standard endoscopic techniques. Due to its safety profile, it can
be indicated in patients with high surgical risk or not eligible to
surgery.
V.02.2
ENDOSCOPIC ULTRASOUND GUIDED RADIOFREQUENCY
ABLATION OF A PANCREATIC NEUROENDOCRINE TUMOUR (WITH
VIDEO)
Armellini E.*, Crinò S.F., Ballarè M., Leutner M., Occhipinti P.
Azienda Ospedaliero Universitaria “Maggiore della Carità”, Novara,
Italy
Background and aim:
The standard of care of pancreatic
neuroendocrine tumours recommends surgical resection of
functioning nodules or of large or high grade non-functioning
ones (>2cm, G2-G3), with relevant costs and post-operative
complications. Local endoscopic ultrasound guided ablative therapy
is described, yet.
Radiofrequency ablation (RFA) is a method to obtain tumour necrosis
by cell protein denaturation induced by tissue heating above 45°C,
applied to treat several malignancies.
Energy is provided by an RFA current generator connected to an
active electrode needle placed into the tumour under imaging
guidance. Induced lesions have variable diameter, depending on
current intensity, active tip length and time.
Recently a novel RFA needle has been developed to be used
under endoscopic ultrasound (EUS) guidance. It is an 18G water
cooled needle, with a 5 to 30 mm long active tip, connected to a
radiofrequency generator (EUSRATM RF Electrode-Viva RF generator,
STARmed, Koyang, Korea).
Material and methods:
A 76-year-old man was referred for a
pancreatic nodule. Labs were within normal ranges. An abdominal
computed tomography (CT) showed an hypervascular 20mm nodule
in the pancreatic tail. EUS-guided fine needle aspiration revealed a
pancreatic neuroendocrine tumour with a Ki67 proliferative index
>5% to yield a G2 grade.
Results:
The patient refused surgical resection and we decided to
treat the lesion by EUS-guided RFA. Under general sedation the
nodule was ablated in a single session, with two passes by a 10mm
long exposed tip needle. The patient remained asymptomatic, with
normal serum pancreatic enzymes and was discharged on the
third day. CT and contrast-enhanced EUS confirmed a complete
radiological ablation on follow-up. No complication was observed
and the patient is disease free to now.


















