
e122
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
V.01.9
ENDOSCOPIC CLOSURE OF IATROGENIC DUODENAL
PERFORATION SUCCESSFULLY TREATED WITH A NEW OVER-THE-
SCOPE CLIP
Anderloni A.
1
, Bianchetti M.*
2
, Di Leo M.
1
, Repici A.
1
1
Istituto clinico Humanitas, Milano, Italy,
2
Istituto clinico Humanitas -
Mater Domini, Castellanza, Italy
Background and aim:
Although rare (0,09%), duodenal perforation is
one of the most critical complication of endoscopic ultrasound (EUS),
with significant morbidity and mortality. With the introduction of
“over the scope” systems, clips and stents, endoscopic management
has become the treatment of choice of the gastrointestinal
perforation in the place of traditional surgical procedures.
Material and methods:
We present a case of a 62-years old man
with jaundice, referred to our unit to undergo EUS-FNA of solid
lesion of pancreatic head followed by ERCP for biliary drainage. The
patient underwent EUS performed with a linear echoendoscope
(GF-UCT140, Olympus Optical Co., Ltd., Tokyo, Japan) under CO2
insufflation and deep sedation with propofol. During the scope
withdrawal in the duodenum, we noticed a full thickness break
of about 13 mm diameter at the upper duodenal knee. Then the
echoendoscope was immediately retrieved.
Results:
With a diagnostic gastroscope loaded with the new OTSC
Padlock Clip (C910001, Aponos Medical Co., Kingston, USA) we
reached the perforation site in the duodenum. The Padlock clip is a
new OTSC device ergonomically designed to be placed on the tip of
the scope without occupying the operative working channel. Since
the diameter of the hole was too wide to be aspirated into the cap,
we used a twin grasper to approach the edges of the perforation
before releasing the OTSC (Video). X-ray with Gastrografin (Bayer
AG, Germany, Leverkusen, Germany) showed the complete closure
of the perforation with no contrast medium leakage. Broad-
spectrum antibiotics were administered intravenously and a CT-scan
performed three hours later confirmed the efficacy of the maneuver.
The patient remained afebrile, asymptomatic with stabile vital
signs. Semiliquid diet was allowed 24 hours later. Three days later,
the patient underwent percutaneous transhepatic cholangiography
and biliary drainage with positioning of a metallic stent. On day 7
postoperatively, the patient was discharged asymptomatic and with
reduction of bilirubin level.
Conclusions:
OTSC is a potentially surgery-sparing device and can
be a useful tool for the immediate closure of duodenal defects. OTSC
should be ready accessible and endoscopist should be trained in
their appropriate use. The Padlock Clip is a new OTSC device readily
deployed, ergonomically designed, that does not occupy a working
channel making the interventional procedure more quick and easy
to perform, with a high technical and clinical success rate.
V.01.10
“DISSECTING THE STONE”: SUCCESSFUL ENDOSCOPIC “LITHO
HYDRO-JET TRIPSY, LHJT” OF A BOUVERET SYNDROME
Staiano T.*
2
, Repici A.
3
, Mutignani M.
4
, Martinotti M.
1
, Rispo A.
5
,
Buffoli F.
6
1
S.C. Chirurgia Generale A.O. Istituti Ospitalieri di Cremona, Cremona,
Italy,
2
S.C. Endoscopia Diagnostica e Chirurgia Endoscopica Fondazione
IRCCS Istituto Nazionale dei Tumori, Milano, Italy,
3
U.O. Endoscopia
Digestiva IRCCS Humanitas, Rozzano, Italy,
4
S.C. Endoscopia
Diagnostica e Interventistica A.O. Niguarda Ca’ Granda, Milano, Italy,
5
DAI Gastroenterologia, Endocrinologia, Chiururgia A.O.U Federico
II, Napoli, Italy,
6
S.C. Endoscopia Digestiva e Gastroenterologia A.O.
Istituti Ospitalieri di Cremona, Cremona, Italy
Background and aim:
Bouveret’s syndrome, is an uncommon
cause for small bowel obstruction. Less than 3% of cases are due
to a gallstone impacted in the duodenum or pylorus resulting in
a gastric outlet obstruction following the passage of a gallstone
from the gallbladder to the duodenum via a cholecystoduodenal
or choledochoduodenal fistula. Most of the successful therapeutic
maneuvers described involve open surgical removal of the stone
through either a gastrotomy or duodenotomy, and reported
morbidity is not insignificant. We report a case of successful
endoscopic removal of a large stone impacted in the duodenal bulb
by means of a modified intracorporeal lithotripsy using hydro-jet
probe connected to an electrosurgical surgical unit.
Material and methods:
An 86 yo woman was admitted to our
hospital for severe epigastric pain, vomiting and nausea. Abdominal
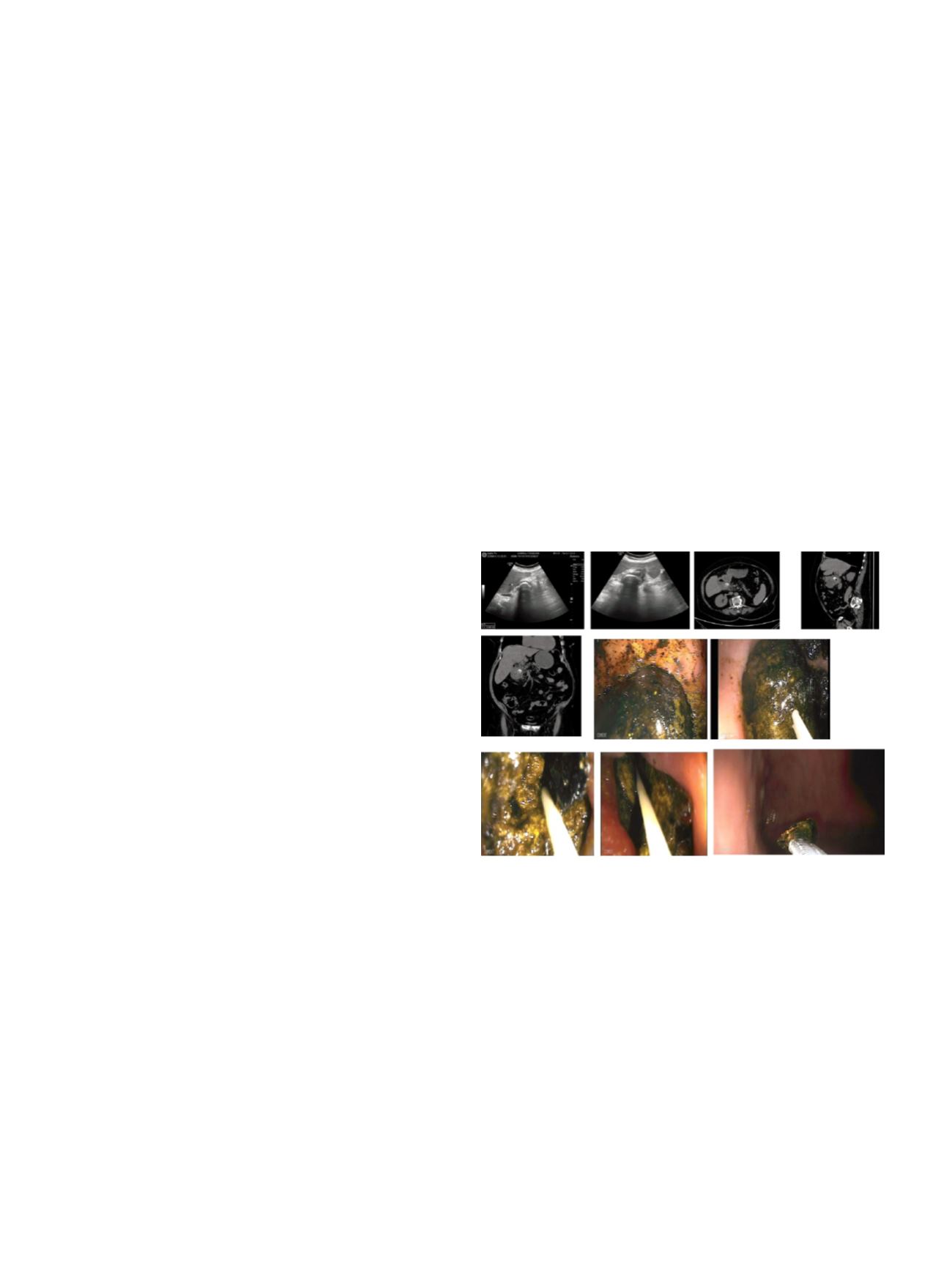
US (Fig 1A) suggested the diagnosis of a biliary fistula and CT scan
detected pneumobilia, a thickened pyloric wall in continuity with
the the gallbladder and stone impacted in the duodenal bulb (Fig. 1
B). EGDs revealed a large (50 x 60 mm) gallstone impacted in the
duodenal bulb (Fig. 1 C), prohibiting passage of the endoscope
downstream. Because of the size and location of the stone,
fragmentation with mechanical lithotripsy was not feasible.
Therefore, we performed intracorporeal endoscopic modified
electrohydraulic lithotripsy using an ERBE JET
®
flexible probe (
∅
1,3
mm; L 2,2 m) for ERBEHydro-Jet connected to electrosurgical unit at
a setting of 50 watts. The probe was advanced through the operative
channel and the cut distal end was applied to the stone for lithotripsy
(Hydro-Jet Lithotripsy, HJL). HJL was repeatedly applied to the stone
with subsequent applications to break the stone into multiple
fragments (Fig. 1 D, VIDEO).
Results:
Loose stone bigger fragments were dragged into the stomach
with a snare, in order to prevent escape into the small bowel with
consequent obstruction of the terminal ileum due to gallstone ileus.
The patient improved clinically. The patient was fully recovered and
was discharged after 6 days of hospitalisation.
Conclusions:
Here, we described the first case of lithotripsy using
an ERBE JET
®
hydro-jet flexible probe for a successful endotherapy
of Bouveret syndrome. The limitation of this method is the risk
involved with inadvertent focusing of the “hydro-jet waves” onto
the surrounding tissue with consequent bleeding and perforation.
Key factors for a successful endotherapy are: excellent stone
visualization, adequate water immersion of the stone, correct
technique (adequate devices handling and electrosurgical setting)
and a skilled endoscopist. In conclusion, endoscopic management
of Bouveret’s syndrome offers an exceptional minimally invasive
option compared to surgery.


















