
e158
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
from baseline. MRI activity was measured by MRI-enterography
global score (MEGS), range 0-296, a score which takes into account
transmural and extramural features, with active disease defined as a
score ≥1, and response as above.
Results:
We enrolled 6M/7F, mean age 36±12 ys, mean disease
duration 7±5 ys. According to the Montreal classification the
phenotype was L1 in 31%, L2 in 7% and L3 in 62%; the behaviour was
B1 in 8%, B2 in 69% and B3 in 23%. Resectional surgery related to CD
was observed in 15%. Signs of mesenteric inflammation were only
lymph node enlargement or comb-sign. 3 patients were treated with
IFX, 10 with ADA (all naive to anti TNF
a
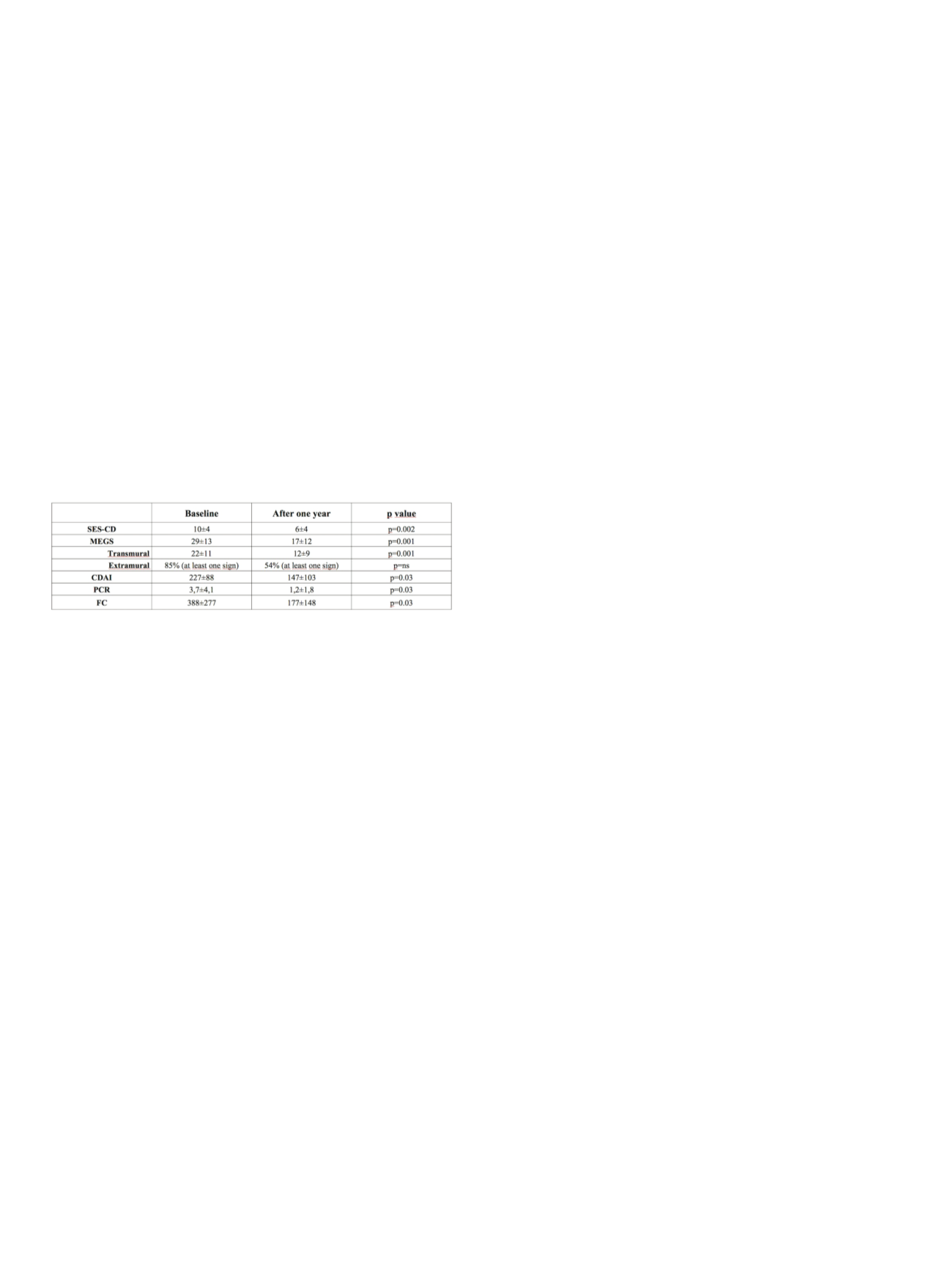
). Mean SES-CD, MEGS, CDAI,
CRP and FC values significantly decreased at one year (table). 53%
had clinical remission, 77% clinical response. Biological remission
was achieved in 69% and 53% according to FC and CRP respectively.
MH was achieved 38%, endoscopic response in 46%. Normalization
of MRI finding was achieved in 15%, 31% had transmural
improvement; before therapy 85% showed at least one extramural
sign of inflammation, after 1 year at least one sign persisted in 54%
(p=ns). MEGS score after one year didn’t change significantly
between patients with endoscopic remission/improvement and
those without (p=0.7). CRP positivity at one year was correlated
with presence of extramural involvement only (p=0.02) and mean
CRP level were higher (2,3 ± 2,4 vs 0,30±0,50 mg/dl) in the presence
of comb-sign (p=0.03).
Conclusions:
Biological therapy is effective in inducing clinical,
biochemical and endoscopical remission of CD while transmural
inflammation may persist longer than one year. Transmural, mainly
extramural, healing probably needs longer therapy to be achieved,
and his activity was unrelated to endoscopic improvement while
closely relates to CRP positivity and levels.
P.07.3
MAINTENANCE OF CLINICAL REMISSION IN IBD PATIENTS
AFTER DISCONTINUATION OF ANTI-TNF AGENTS, AN ITALIAN
EXPERIENCE
Monterubbianesi R.*
3
, Furfaro F.
2
, Costantino G.
1
, Bezzio C.
2
,
Giannarelli D.
4
, Fries W.
1
, Maconi G.
2
, Kohn A.
3
1
Dipartimento di Med Interna, Università di Messina, Messina, Italy,
2
Dipartimento di Gastroenterologia, Ospedale Universitario L.Sacco,
Milano, Italy,
3
UO Gastroenterologia, AO San Camillo Forlanini, ROMA,
Italy,
4
U.dibiostatistica, Ospedale Regina Elena, Roma, Italy
Background and aim:
Despite the long experience in the treatment
of Inflammatory Bowel Disease (IBD) with antiTNF agents, we still
don’t know whether and when stopping the biological treatment
in patients that are in clinical remission. Aim of our study was to
assess the risk of relapse in an Italian cohort of IBD patients who
discontinued antiTNF therapy because of clinical benefit and to
evaluate if the mucosa healing is associated to a better outcome.
Material andmethods:
Consecutive patients followed in three Italian
referral center for IBD, affected by Crohn Disease (CD) or Ulcerative
Colitis (UC), and who received an antiTNF agent, infliximab (IFX)
or adalimumab (ADA) for a period ≥12 months and discontinued
the drug because in clinical remission, were included. All patients
had an endoscopy performed before and after the treatment with
antiTNF. Demographic, clinical and endoscopic characteristics of
patients were collected. Relapse was defined as need for rescue
therapy (corticosteroids or new cycle of antiTNF) or surgery.
Results:
126 patients were included, 99 were affected by CD (78.6%)
and 27 by UC (21.4%). Median age was 35 years old (range 15-78yrs).
56% were male. 29.4% of patients underwent surgery in the past. 108
patients received IFX (85.7%) and 18 ADA (14.3%). A concomitant
treatment with immunosuppressant therapy (ISS) was seen in 65.9%
of patients. Mucosal healing was achieved in 77 patients (61.6%).
Kaplan-Meier curves showed a cumulative probability of a disease
free course at 1 year of 78%. After 2 years from stopping antiTNF 64%
of patients were on remission. Probability of relapse after 5 years
was 54%. In the univariate analysis, the following variables resulted
related to the probability of mantenaince clinical remission:
gender (male, 0.001), age (>=35 ys, 0.05), and concomitant
immunosuppression (0.02). Mucosa healing was not associated to
a better outcome.
Conclusions:
In our cohort, composed by IBD patients treated with
antiTNF at least for 1 year, who discontinued the treatment because
in clinical remission, the probability to maintenance clinical benefit
at 2 years was 64%. Risk of relapse was more frequent in the first
2 years from withdrawal. healing was not associated to a better
outcome in our cohort. Prospective studies are needed to identify
patients with a low risk to relapse.
P.07.4
HEMOGLOBIN AND FERRITIN VALUES ARE ASSOCIATED WITH
INCREASED RATE OF MUCOSAL HEALING IN PATIENTS WITH
CROHN’S DISEASE TREATED WITH ANTI-TNF ALPHA
Mendolaro M.*, Cappello M., Viola A., Cilluffo M.G., Vita G.,
Peralta S., Calvaruso V., Craxi A.
Gastroenterology Section, DiBiMis, University of Palermo, Palermo,
Italy
Background and aim:
In the era of biologics, mucosal healing
(MH) has become a relevant treatment goal in inflammatory bowel
disease (IBD), since it is associated with a lower rate of relapse,
hospitalization and surgery. In this study, we aimed to evaluate rate
and predictive factors of MH in a homogeneous cohort of Sicilian
patients with Crohn’s disease (CD) treated with anti-TNF agents.
Material and methods:
We report data of 43 consecutive patients
with Crohn’s disease (CD), treated with anti-TNF alpha at our IBD
clinic from January 2012 to September 2015. Clinical-demographic
characteristics (sex, age, smoking habits, familial predisposition,
disease location and behavior (Montreal), activity (Harvey–
Bradshaw Index [HBI]), indications to biologic therapy, concomitant
medications, and serum biomarkers (CRP, haemoglobin [Hb],
ferritin) were registered on a dedicated database. Each patient
underwent ileocolonoscopy at the beginning of treatment and after
12 months. Simple Endoscopic Score for Crohn’s Disease (SES-CD)
was used to assess endoscopic activity. Mucosal healing was defined
as a SES-CD score between 0 and 3.
Results:
Mean duration of CD of the 43 patients (22 males; mean
age 43,9 ± 14,2 years) was 126 ± 77 months. Thirty-two patient
were treated with adalimumab (74%) and 11 with infliximab (26%).
Mucosal healing was observed in 25 patients (58%). Infliximab
achieved a higher, though not significant, endoscopic response
rate as compared to adalimumab (88% vs 50% p= 0.065). Clinical
remission (HBI <5) was obtained in all patients with MH and in 13
of 18 patients that didn’t get it (100% vs 72%, p=0,005). No difference
concerning duration, extent, behavior was detected. Mean Hb values
at baseline (13.3 ± 1.2; p=0,023) and after 12 months (13,7 ± 1.2;
p=0,05) were higher in patients who obtained MH. Ferritin values
>30 ng/ml was significantly more frequent in patients with MH, both
at baseline (p=0,030) and after 12 months (p=0,017). No significant
difference as far as concerns CRP was found.


















