
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e159
Conclusions:
As previously reported, biologics induce endoscopic
response at 12 months in more than 50% of patients with CD.
Disease features did not predict MH. Hemoglobin and ferritin were
the only laboratory parameters significantly related to MH, while
no significant difference was observed for CRP. Our results could
suggest to use these parameters to drive timing of endoscopic
reassessment in patients with CD on biological therapy.
P.07.5
ON THE ORIGIN OF CRP IN CROHN’S DISEASE: ROLE OF THE
EXTRAMURAL COMPONENT
Serio M.*
1
, Pierro A.
2
, Efthymakis K.
1
, Laterza F.
1
, Maselli G.
2
,
Milano A.
1
, Bonitatibus A.
1
, Sallustio G.
2
, Neri M.
1
1
Medicine and Aging Sciences and CESI,, Università “G. D’Annunzio”,
Chieti, Italy,
2
Radiology Department, Fondazione di Ricerca e Cura
“Giovanni Paolo II’’, Università Cattolica del Sacro Cuore, Campobasso,
Italy
Background and aim:
Due to the full thickness involvement of the
bowel wall or complications, Crohn’s disease (CD) evaluation is
the result of an integration of endoscopy (the gold standard) with
clinical, laboratory and radiological data. The role of MRI, which
excels in identyfing extramural signs of inflammation, is still unclear
in CD follow-up. Moreover it is still debated whether CRP serum
levels increase is due to mucosal or mural/extramural inflammation,
not only via liver production but also from extrahepatic sources such
as of the mesenteric fat hypertrophy (MFH), a CD common feature,
which assessed by CT was found to correlate with plasma CRP
levels in CD patients. Aim was to correlate enteric and extraenteric
inflammatory MRI findings with endoscopic severity and CRP in a
group of CD patients.
Material and methods:
52 consecutive patients with endoscopically
proven CD underwent MRI enterography for the staging at diagnosis
or activity assessment (68/32%). Endoscopic activity was scored
through the SES-CD (range 0-40) with active mild, moderate ad
severe disease defined as 4-10, 11-19 and >20 respectively. MRI
activity was scored through the MEGS score (range 0-296), which
integrates both mural and extramural items, namely lymph node,
fistula, abscess and comb sign, with active disease defined as ≥ 1
score. For all participants CDAI was completed and CRP and fecal
calprotectin (FC) were measured (positivity cut-off respectively
>0,50mg/dl and >150μg/gr). MFH was qualitatively defined a bowel
loop separation ≥ 3 cm.
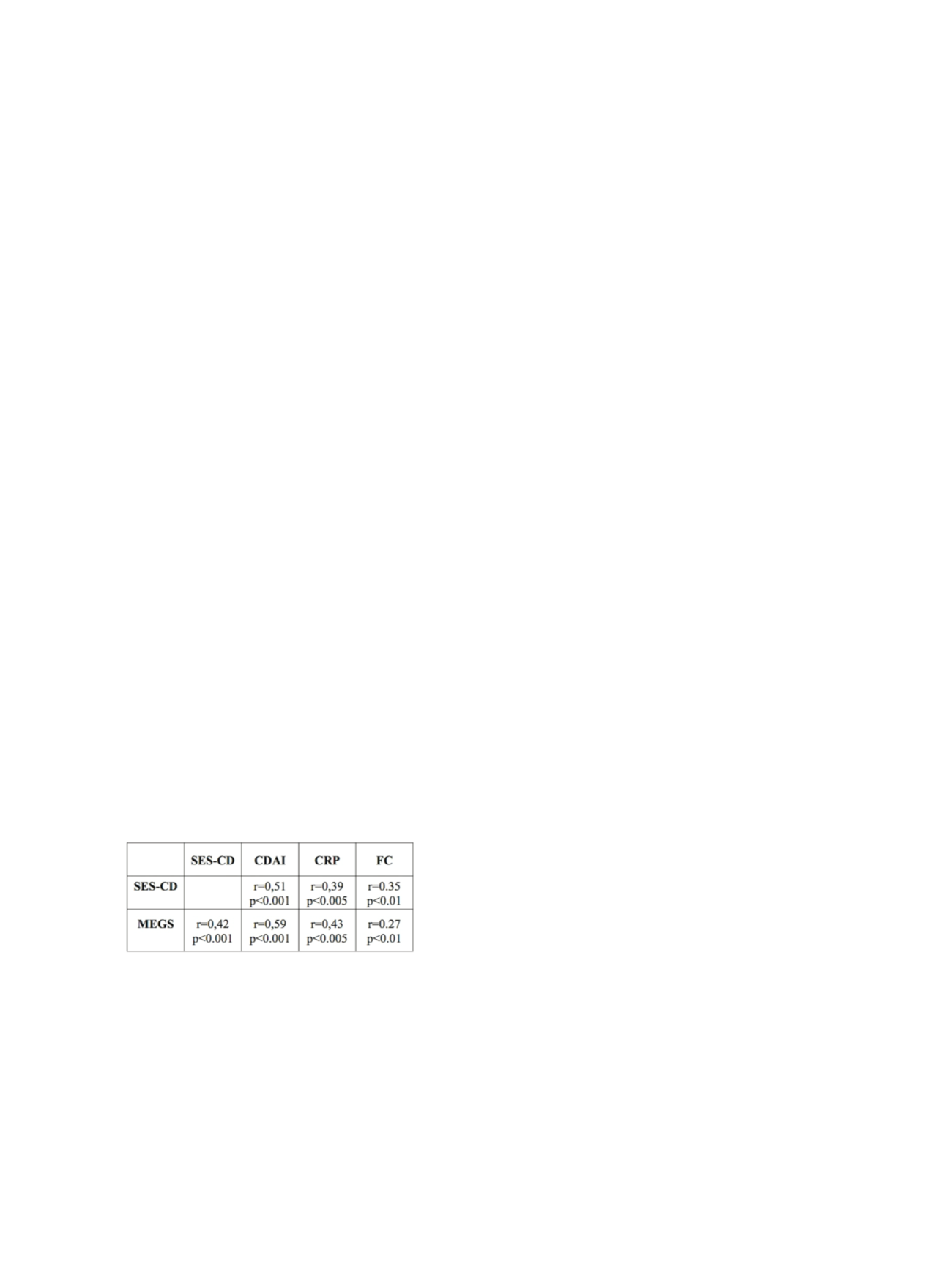
Results:
We enrolled 20M/32F, mean age 38±15 ys, mean CD duration
5±5 ys. SES-CD and MEGS correlated well between them and with
clinical and biological activity (table). According to SES-CD 62% of
patients had mild, 19% moderate and 5% severe disease. Increasing
severity at endoscopy was significantly correlated with trasmural/
extramural involvement, only with CRP positivity (p=0.007). MRI
did not show ability to distinguish endoscopic severity (p=0.14),
but revealed trasmural/extramural signs of inflammation in 60% of
patients in remission, 84% mild and 100% with moderate and severe
disease, mostly with CRP positivity. Moreover CRP positivity was
associated with the presence of extraintestinal (p=0.006; lymph
nodes p=0.009, combsign p=0.001 and abscess p=0.005), not of
mural involvement (p=0.4). Mean CRP levels increased according to
the number of extramural signs of inflammation (from absence to 4
signs p=0.01). Patients with MFH showed higher levels of CRP than
those without (4,2±4 mg/dl vs 1,9±3,2 p=0.005).
Conclusions:
Transmural inflammation, which is more frequent
in severe disease, may still be present regardless of endoscopical
activity. Positive CRP is significantly correlated to extramural activity
in CD patients, thus suggesting the need of MRI for the staging of the
disease independently from endoscopic severity. Moreover these
data suggest that mesenteric fat may contribute to the increased
CRP production
P.07.6
ROLE OF DIFFUSION-WEIGHTED IMAGING (DWI) IN MRI-
ENTEROGRAPHY FOR THE EVALUATION OF SURGICAL RISK IN
PATIENTS WITH CROHN’S DISEASE
Rispo A.*
1
, Mainenti P.
2
, Musto D.
1
, Testa A.
1
, Imperatore N.
1
, Rea M.
1
,
Nardone O.M.
1
, Taranto M.L.
1
, Castiglione F.
1
1
Gastroenterology “Federico II” University, Naples, Italy,
2
Radiology
“Federico II” University, Naples, Italy
Background and aim:
In Crohn’s disease (CD) it’s useful to
discriminate inflammatory from fibrotic lesions. MRI-Diffusion
Weighted Imaging (DWI) is able to identify active inflammation in
most pathological tissues.
Aim:
To define the role of DWI sequences
in the evaluation of the risk of surgery in patients with CD.
Material andmethods:
FromMarch 2011 to June 2013 we performed
an observational prospective study including all consecutive CD
patients with active disease undergone a MRI-enterography. MRI
study included: measurement of bowel wall thickness (BWT), CD
extension, enhancement pattern, pre-stenotic dilation, presence
of oedema and/or comb-sign, presence of fistulas/abscesses, (T2
weighted, T1-weighted gadolinium-based contrast material uptake).
Furthermore, all patients were studied by DWI sequences defining:
visual analysis of iperintensity corresponding to a qualitative value
of reduction of diffusion on a scale (0-4), quantitative analysis of
Apparent Diffusion Coefficient (ADC) maps (max, min and medium).
The medical/surgical treatments during the following 12 months
were also recorded. Statistical analysis was performed dividing all
patients in 2 groups (operated vs not operated) using T-student test
for continue variables and X-square test for dichotomic variables.
To identify the variables associated to surgical risk, we performed
a logistic multiple regression expressing the risk in terms of Odd
Ratio. A p value lower of 0.05 was considered significant. Finally, the
diagnostic accuracy was tested by a ROC curve.
Results:
110 patients (61M/49F) were enrolled in our study (median
age 37,6 years) and 127 bowel segments resulted pathologic at
MRI. 26 patients (23,6%) and 31 segments were resected during the
follow-up period. At all pathological segments, the iperintensity in
DWI sequences, the reduction of ADC max, ADC medium and the
presence of fistulas/abscesses were significantly associated with
a subsequent surgical intervention (p<0.05). In particular, the
presence of CD complication was the variable with the highest risk
of surgery (p=0.08; OR 3.9; 95% CI 1,4-10,7). When excluding the
patients with complications, we reported a significant correlation
of DWI iper-intensity, ADC max and medium with surgical
intervention. Interestingly, the reduction of ADC medium was the
variable with the highest risk of surgery (p=0,03; OR 2.0; 95% CI
0,79-0,92). The cut-off value for discriminating patients at risk of
surgery was 1,081x10-3 mm2/s (sensibility 55.6%, specificity 70.3%,
PPV 33.3%, NPV 85%).
Conclusions:
The presence of fistulas/abscesses remains the
variable most associated with surgical risk in CD. In not complicated
CD, the evaluation of DWI sequences at MRI-Enterography, and in
particular the reduction of ADC medium, correlates with the need
of surgery. High value of ADC medium shows high NPV for surgery
in CD patients.


















