
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e165
of the paucity of data in this regard. We aimed to investigate the role
of IBP in consecutive patients with esophageal symptoms.
Material and methods:
We included consecutive patients with
esophageal symptoms referring to our motility laboratory. Patients
with gastro-intestinal surgery, achalasia or scleroderma were
excluded. All patients underwent esophagogastroduodenoscopy
(EGDS) and HRM with 5-min baseline recording and 10 single
water swallows. The diagnostic criteria agreed with the Chicago
Classification vers. 2. We stratified these patients according to their
IBP value (i.e. normal if lower than 17mmHg) in two groups: patients
with and those with abnormal IBP values. Data were expressed as
mean and standard deviation. A t-test and x2-test were performed
and a p-value <0.05 was considered statistically significant.
Results:
Patients with abnormal IBP had a mean age higher
than patients with normal IBP (60±13 vs 50±16; p value <0.001),
but no difference was found in gender distribution. As to HRM
characteristics, patients with abnormal IBP had similar mean
Distal Contractile Integral (DCI) than those with normal function
(2287±10538 vs. 2100±1497; p=0.9), but a lower LES resting pressure
(22±11vs 33±16; p<0.001) and an increased IRP (22±11vs33±16;
p<0.001). No differences in terms of distal latency (6.7±1.5% vs
6.4±2.0%; p=0.14), peristaltic swallow (70±34% vs 78±27%; p=0.07)
and abnormal type of swallow such as failed, ineffective, and
fragmented (p=ns).
Conclusions:
Abnormal IBP values correlate more with EGJ
dysfunction rather than with vigor of peristalsis suggesting that EGJ
compliance plays a major role in its determination. This association
is further supported by the increased age of patients with abnormal
IBP (i.e. known fibrotic alterations related to aging).
P.08.2
PROXIMAL GASTRO ESOPHAGEAL REFLUX: WHAT’S WRONG
WITH GASTRO-ESOPHAGEAL MOTILITY?
Consalvo D.*
1
, Pescador D.
1
, Stefani N.
1
, Sozzi M.
1
, Simeth C.
1
,
Tonello C.
1
, Paolini A.
1
, Fabro M.
1
, Urban F.
1
, Leandro G.
2
, Monica F.
1
1
Azienda Ospedaliero Universitaria “Ospedali Riuniti”, Trieste, Italy,
2
IRCCS De Bellis, Castellana Grotte (BA), Italy
Background and aim:
Atypical symptoms are common in gastro-
esophageal reflux disease (GERD). Multichannel intra-luminal
impedance and pH monitoring (MII-pH) give information about
GERD and esophageal activity. Less than 40% of patients with
suspected laryngo-pharyngeal reflux has a diagnosis of GERD but
little is known about the pathogenesis of proximal extent of GERD.
Aim:
to assess the correlation between proximal extent of GERD,
esophageal activity and dyspeptic symptoms (nausea, belching,
postprandial fullness).
Material and methods:
Fifty patients, 26 women, aged between 22
and 83 years old with a diagnosis of NERD and atypical symptoms
underwent MII-pH, after a negative upper endoscopy. All patients
were PPI-off and H. pylori infection, autoimmune diseases and non-
obstructive dysphagia were excluded.
Results:
Sixteen patients (32%) had a MII-pH tracing compatible
with proximal extent of reflux. There was a positive correlation
between number of episodes of reflux and proximal reflux (
ρ
=
0.852). Patients with proximal extent of reflux had a median bolus
clearance time delayed (75%vs 41.2%, p= 0.03) and the presence of
dyspeptic symptoms (56.3%vs20.6%, p = 0.01). No difference was
ruled out for acid refluxes (p = 0.16), weakly acid refluxes (p = 0.88),
upper symptoms (p = 0.73) and Symptom Association Probability
(p = 0.33).
Conclusions:
Patients with atypical symptoms and proximal extent
of GERD had a reduced esophageal clearance associated with a
possible delayed gastric emptying. More studies are needed to
identify different subgroups of patients for tailoring therapy.
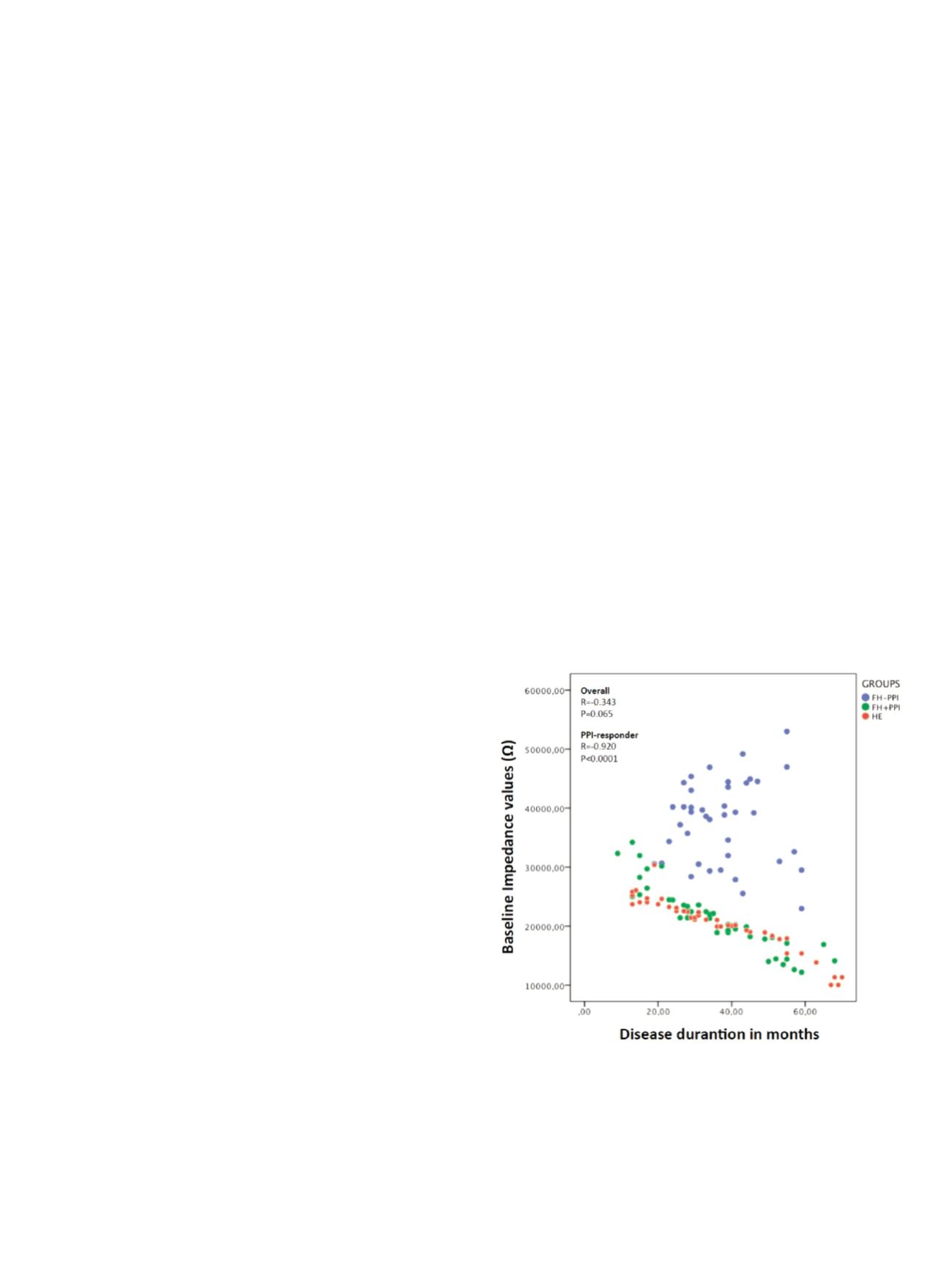
P.08.3
BASELINE IMPEDANCE VALUES CAN REPRESENT A MARKER OF
GASTROESOPHAGEAL REFLUX DISEASE AND ARE STRONGLY
RELATED WITH THE DURATION OF THE DISEASE
Bertani L.*
1
, De Bortoli N.
1
, Russo S.
1
, Martinucci I.
1
, Furnari M.
2
,
Tolone S.
3
, Frazzoni M.
4
, Frazzoni L.
4
, Ricco G.
1
, Fani B.
1
,
Mumolo M.G.
5
, Costa F.
5
, Savarino V.
2
, Marchi S.
1
, Savarino E.
6
1
University of Pisa, Pisa, Italy,
2
University of Genoa, Genoa, Italy,
3
Second University of Naples, Naples, Italy,
4
Baggiovara New
Hospital, Modena, Italy,
5
Az. Ospedaliero-Universitaria Pisana - UO
Gastroenterologia Univ., Pisa, Italy,
6
University of Padua, Padua, Italy
Background and aim:
Recently, it has been described a strong
correlation between baseline impedance (BI) values and the
symptom relief during proton pump inhibitor treatment. The aim
of the study was to evaluate BI levels in patients with heartburn
responder and non-responder to acid suppressive therapy (PPI) and
to detect the relationship between BI values and number of months
of GERD-related symptoms.
Material and methods:
NERD patients with heartburn were
enrolled and asked to indicate from how long they experienced
heartburn (i.e. disease durantion in months). All patients underwent
24-h impedance-pH test off-PPI therapy and we selected those with
normal acid exposure (AET) and number of reflux events. Thus, 90
patients undertook an 8-week course of PPIs. Sixty of them with
>50% symptom improvement were classified as PPI-responders: 30
patients with pathophysiological characteristics of functional
heartburn (negative symptom-reflux correlation; FH+PPI) and 30
with hypersensitive esophagus (positive symptom-reflux corre
lation; HE). The remaining 30 patients with a <50% improvement to
treatment and with pathophysiological characteristics of functional
heartburn were classified as PPI non-responders (negative reflux
symptom correlation; FH-PPI). BI value were calculated manually
during overnight rest.
Results:
The mean duration of symptoms (in months) was not
different between FH+PPI (34.1±15.4), HE (35.7±17.8) and FH-PPI
(36.5±15.5); p=ns. Patients with FH+PPI showed a higher mean
AET (1.9%±1 vs 0.6%±0.6, p<0.05), mean reflux number (30.4±9.3 vs
23.5±7.9, p<0.05) and acid reflux number (17.1±8 vs 10±6.9, p<0.05)
compared to FH-PPI. Patients with HE showed mean AET (2.3%±1.8)
and total reflux number (34.6±10.4) similar to those recorded in
FH+PPI (p=ns). Baseline impedance levels were lower in FH+PPI


















