
e166
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
(1949.6±548.8) and in patients with HE (1839.7±467.6) than in FH-
PPI (3812.8±810.2) (p<0.001). The overall correlation between BI and
disease duration in months was poor (r=-0.343; p=0.065) but when
we evaluated the patients who responded to PPI (HE and FH+PPI) we
found a very strong correlation between baseline value and duration
of the disease (r=-0.920; p=0.0001).
Conclusions:
Our results showed a very strong correlation between
lower BI and response to PPI treatment. BI could represent a marker
of GERD. We also found a strong negative correlation between
BI values and disease duration in PPI-responder patients, thus
corroborating the relevance of this objective marker in evaluating
the esophageal mucosal impairment.
P.08.4
INCIDENCE AND MANAGEMENT OF ACHALASIA IN CLINICAL
PRACTICE: AN EIGHT-YEAR SINGLE CENTRE EXPERIENCE
Michielan A.*, Betetto G., Lamboglia F., Cappuccio R., Bortoluzzi F.N.,
Pallini P., Caroli A.
Ospedale dell’Angelo-Ospedale SS. Giovanni e Paolo, Mestre-Venezia,
Italy
Background and aim:
Achalasia is a relatively uncommon primary
esophageal motility disorder. Its incidence in clinical practice has
not been established yet and the gold standard of treatment is
still debated. The aim of this study was to report the incidence of
achalasia in our region (Azienda ULSS 12 Veneziana, Veneto Region,
North-East of Italy) and to evaluate the modalities and outcome of
treatment according to the clinical characteristics of patients.
Material and methods:
We retrospectively evaluated our
manometric records from January 2008 to September 2015. All
patients with a new diagnosis of achalasia were classified into one
of the three groups of the Chicago manometric classification. The
subsequent modalities and outcome of treatment were recorded.
The options of treatment included surgical miotomy (SM),
pneumatic dilatation with Rigiflex balloon (PD) or Botox injection
(BI). Symptoms relapse after PD was identified by an Eckardt Score
>3, and treated with repeated PD sessions as required.
Results:
46 patients were diagnosed in eight years (M/F 27/19;
median age 62, IR 46.75-68.75), with a mean incidence of 2/100000
per year. Type II was the most frequent subtype of achalasia (32
patients, 69.57%) whereas type I and III were rarer (6 patients –
13.04% - and 8 patients – 17.39% - respectively). The manometric
presentation was not affected by gender or age class (< 50, 50-70
or > 70 years) as confirmed by the Fisher Exact Test (p = 0.955 and
p=0.905 respectively).
11 patients were lost after the diagnosis because they were treated
in other centres and 4 patients had only mild symptoms which were
controlled by dietary and behavioral changes. 7 patients underwent
SM as the primary treatment, and 2 after failure of endoscopic
techniques (1 BI and 1 PD). None of them had a symptomatic
relapse. 22 patients were successfully treated with PD: 10 patients
had only one session (45.45%), 8 patients two sessions (36.36%), 3
patients three sessions (13.64%) and 1 patient 4 sessions (4.55%). No
complications were reported. A binary logistic model for multiple
variables was used to identify any factors related to PD outcome:
gender, age class and manometric subtype were tested. Older age
was a protective factor for repeated dilatations (OR 0.146, 95% CI
0.025-0.870, p = 0.035).
Conclusions:
The incidence of achalasia in our region is stable in the
last eight years and slightly higher than previously reported. Type
II is the most frequent subtype, regardless gender and age. PD is a
safe procedure which may require repeated sessions, particularly in
younger patients.
P.08.5
FEASIBILITY OF HIGH RESOLUTION IMPEDANCE MANOMETRY IN
ASSESSING BARRETT’S ESOPHAGUS EXTENSION
Furnari M.*
1
, Tolone S.
2
, Savarino E.
3
, De Bortoli N.
4
, Frazzoni M.
5
,
Martinucci I.
4
, Marchi S.
4
, Savarino V.
1
, Marabotto E.
1
, Zentilin P.
1
1
Departement of Internal Medicine, Gastroenterology Unit, University
of Genoa, Genoa, Italy,
2
Division of Surgery, Department of Surgery,
Second University of Naples, Naples, Italy,
3
Division of Gastroenterology,
Department of Surgery, Oncology and Gastroenterology, University
of Padua, Padua, Italy,
4
Division of Gastroenterology, Department
of Internal Medicine, University of Pisa, Pisa, Italy,
5
Division of
Gatroenterology, Baggiovara Hospital, Modena, Italy
Background and aim:
Diagnosis and surveillance of Barrett’s esopha
gus (BE) is performed by means of upper endoscopy with biopsies,
which is also important to assess the extension of metaplasia. Several
studies demonstrated the risk of dysplasia and adenocarcinoma
development in BE is associated to its extension. However, endoscopic
evaluation of esophago-gastric junction (EGJ) may be inaccurate,
especially in patients with hiatal hernia, reflux esophagitis and
abnomal z-line. Recent studies carried out with 24-h impedance-pH
testing showed that Barrett mucosa is characterized by very low basal
impedance values compared to the normal esophageal epithelium.
High resolution impedance manometry (HRiM) is able to localize
with more accuracy than upper endoscopy the EGJ and, also, has been
recently applied for baseline impedance levels (BI) in patients with
reflux disease. We aimed to assess Barrett extension by means of BI
assessed by HRiM using upper endoscopy as reference standard. In
contrast, HRiM was considered reference for EGJ evaluation.
Material and methods:
Consecutive patients with proven BE
and a group of healthy volunteers (HVs) were enrolled. Patients
underwent endoscopy and HRiM before imp-pHmetry off-PPI
therapy was performed. BE extention was endoscopically assessed
according to Prague classification. During HRiM, EGJ has been
identified by assessing the position of lower esophageal sphincter
and diaphragm. BI was recorded every cm above the EGJ. Maximal
length (M) at endoscopy was used for comparison.
Results:
Ten HVs (4M/6F; 35yy, BMI 23) and 20 BE patients (11M/9F;
46yy, BMI 25.9) were enrolled. Among BE, hiatal hernia (HH) was
found in 15 pts (75%) during endoscopy and 12 (60%) with HRiM.
Endoscopy overestimated HH of at least ≥1cm in 9 cases. Mean HH
was 1.7 vs0.9cm, respectively (mean error 0.75 cm, median SD:0.25;
r:0.78). HVs had no HH. Median BE length was 1.7cm (1.5-2.3) at
endoscopy, whereas was 2cm (1.0-3.5) at HRiM (median SD
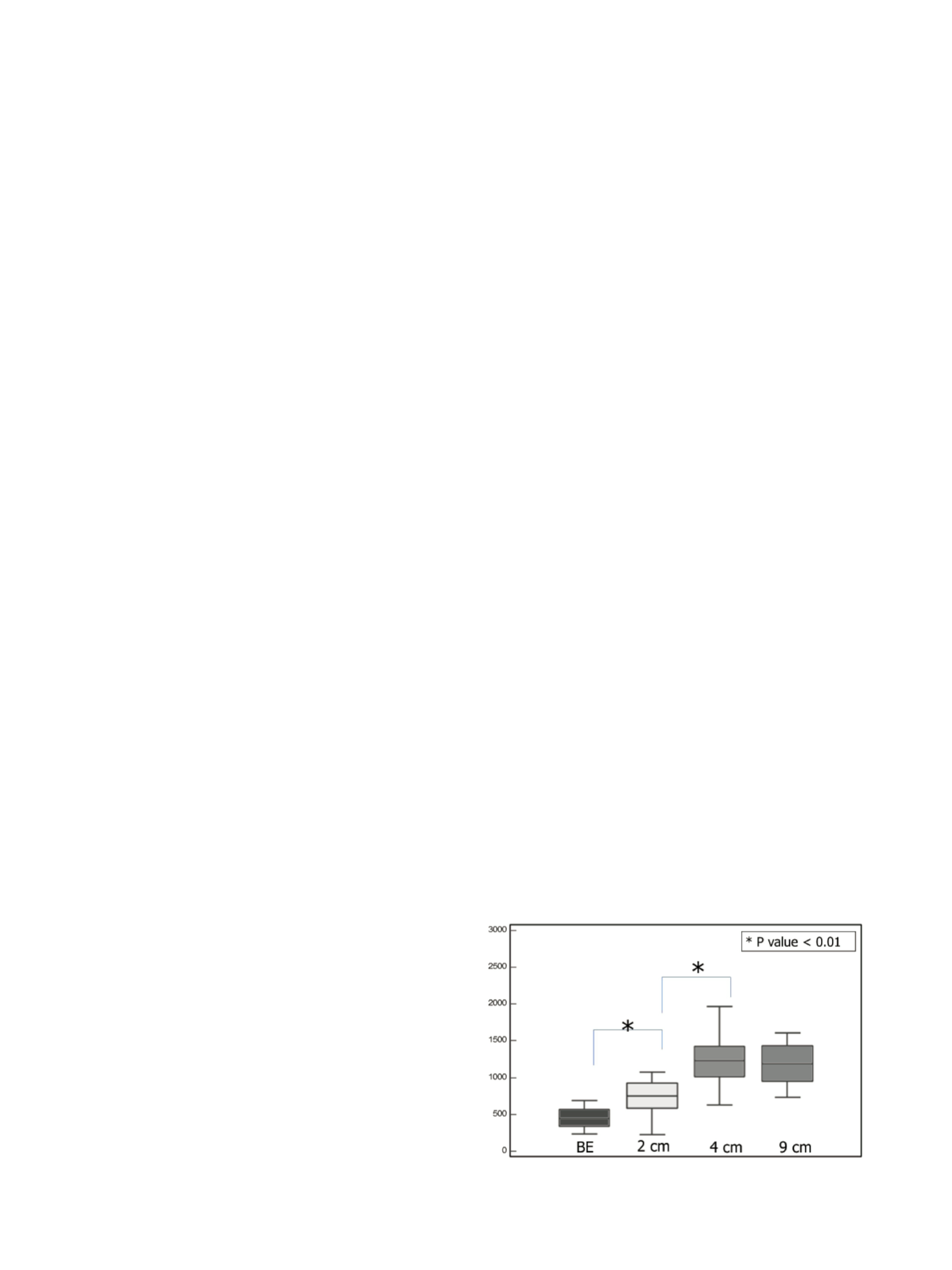
error:1cm; r:0.32). During HRiM BE mucosa showed lower BLI
compared to HV (p<0.01). Median BI of Barrett segment was lower
compared to BI of normal mucosa measured in the same patients
(430
Ω
vs 650
Ω
at 1 to 3 cm above BE, vs 1077
Ω
at 4 to 7cm above BE;
p<0.01). AUC 0.89; BLI of 650
Ω
provides Sens 95.6% and Spec 80.0%.
Fig. 1.
BLI measured at the site of Barrett’s esophagus and at 2-4-9 cm from the upper
limit of BE.


















