
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
e181
measured by the (51)Cr-EDTA permeability test. Only patients at the
first episode of SBP and HE were included.
Results:
Thirty-two cirrhotic patients (Child-Pugh A 10/B 11/C 11;
median MELD score 15) were included in the analysis, 16 of them
experiencing a complication (4 HE, 7 SBP, 5 both) and 16 who did not
being controls. According to receiving operator curve (ROC; Figure
1), the accuracy in predicting the development of complications
was: IP 84.4% (95%CI 0.672- 0.947), MELD 89.5% (95%CI 0.735-0.975),
CHILD 79.5% (0.616-0.916), without any statistical difference (IP vs
MELD p=0.450; IP vs CHILD p=0.190).
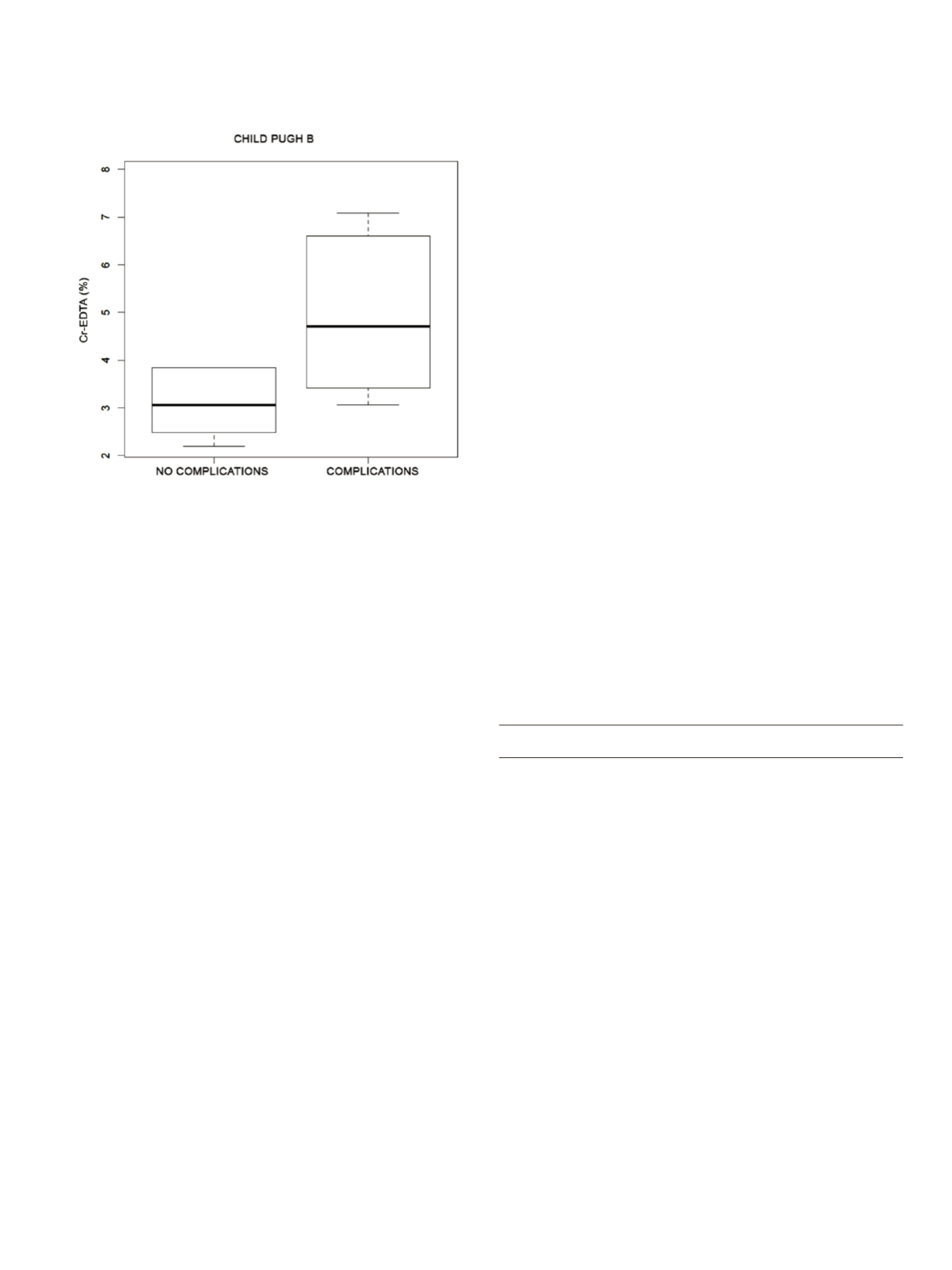
Altough median IP was directly correlated with MELD (Spearman’s
rho 0.564, p<0.0001) and Child-Pugh scores (Spearman’s rho 0.637,
p<0.0001), in case of moderate liver impairment (Child-Pugh B)
it was able to discriminate between patients who developed a
complication and those who did not (Figure 2). As expected, all
patients with Child-Pugh C showed a high IP independently of
complications.
Conclusions:
IP accuracy is comparable to Child Pugh and
MELD scores in predicting the development of liver cirrhosis
complications. However, among patients with moderate liver
impairment, high values of IP allow to identify those more prone to
develop complications.
P.10.10
FEASIBILITY OF HCV INFECTION SCREENING IN BABY BOOMERS
WITH A RAPID, NON-INVASIVE POINT-OF-CARE TEST IN ORAL
FLUID
Blume J.F., Simone L.*, Boccia S., Trevisani L., Pazzi P.
Department of Gastroenterology, S. Anna Hospital, Ferrara, Italy
Background and aim:
The overall prevalence of anti-HCV positivity
in Italy is about 3.2% with a remarkable north-south gradient,
depending on the age of the population being analyzed. In some
southern region where the prevalence of anti-HCV is over 12%
overall, the rate among persons younger than 30 years of age is only
1.3% compared to 33.1% in subjects older than 60 years. According
to the U.S. Department of Health and Human Services most cases
of HCV infection worldwide are currently undiagnosed. People born
from 1945 through 1965, so called “Baby Boomers”, are five times
more likely to have HCV. The longer people live with HCV the more
likely they are to develop serious liver disease like cirrhosis and liver
cancer. Furthermore HCV related complications represent a major
item of expenditure for the National Health Service. In recent years
you can notice a growing demand to launch a nationwide quality-
assured HCV screening program targeted especially at individuals
born between 1945 and 1965. The aim of the current pilot study was
to screen a group of 50 asymptomatic individuals born between 1945
and 1965 with a non-invasive rapid antibody test for the detection of
IgG HCV antibodies.
Material and methods:
We used the OraQuick/HCV Rapid Antibody
Test (OraSure Technologies), a rapid immunoassay for the detection
of IgG HCV antibodies in oral fluid, whole blood, serum and plasma
specimens, giving results in 20–40 minutes. To reduce patient
disconfort we choose to take oral fluid samples from buccal mucosa.
According to recent studies sensitivity and specificity of the oral
fluid test version are 97.8%. The test has been offered for two weeks,
costless, to all our outpatients between 50 and 70 years of age
attending for endoscopic procedures. Volunteers with known HCV
infection were excluded a priori.
Results:
52 volunteers (med age 61.7 years) without known HCV
infection have been tested for IgG HCV antibodies during our 2-week
screening program; 29 were female (med age 61.4 years) and 22 male
(med age 62.0 years). 3 tests, all in patients with atrophic gingiva,
had to be interpreted as invalid since no control line appeared in the
test window. All participants have been found non-reactive for the
presence of IgG HCV antibodies in oral fluid.
Conclusions:
Even though all evaluable 49 participants were
found to be negative for HCV antibodies in oral fluid, we consider
the performance of a national HCV screening program useful to
identify patients with asymptomatic infection. The progression of
HCV disease usually occurs over decades and HCV complications
represent a significant item of expenditure for the National Health
Service. A screening program can help to identify the disease at an
early stage and get people into lifesaving treatment. We consider the
use of a rapid, non-invasive point-of-care test, which can be used
either with venous blood, finger stick blood, serum, plasma or oral
fluid, a good screening tool to realize HCV screening, especially in
non-clinical settings.
P.11 Endo/EUS 2
P.11.1
EUS-GUIDED PANCREATICOGASTROSTOMY AFTER GASTRIC
SURGERY WITH ROUX-EN-Y RECONSTRUCTION: A BRIEF CASE
SERIES
Sica M.*, Manta R., Tringali A., Forti E., Dioscoridi L., Pugliese F.,
Mutignani M.
Surgical Digestive Diagnostic and Interventional Endoscopy, “Niguarda
Ca’ Granda Hospital”, Milano, Italy
Background and aim:
Altough surgical drainage of the pancreatic
duct is considered more effective than endoscopic treatment in
patients with obstruction of the pancreatic duct due to severe
chronic pancreatitis, surgery is not always eligeable. In these
cases, endoscopic procedures can be chosen in order to resolve the
symptoms.
Material and methods:
Three patients presented with upper
abdominal pain due to chronic pancreatitis. All patients
underwent gastric surgery with Roux-en-Y reconstruction.
Transpapillary access was not possible and EUS was used to perform
pancreaticogastrostomy (PGS).
Results:
EUS-guided PGS was performed in all cases. No technical
complications were recorded. The postoperative course was
characterized by mild abdominal pain and hyperamilasemia in the
patient with previous pancreaticoduodenectomy; it was uneventful


















