
e148
Abstracts of the 22
nd
National Congress of Digestive Diseases / Digestive and Liver Disease 48S2 (2016) e67–e231
new endoscopy performed 6 months later confirmed the varices.
An upper gastrointestinal endoscopy showed no evidence of
esophageal, gastric varices.
Material and methods:
In 11/2014 he was admitted for further
evaluation. He reported recurrent abdominal pain, denied other
episodes of hematochezia. He declared to smoke 10 sigarettes qd, no
alcohol abuse ore illicit drug use was noted. Both his father and his
grandfather died for a colon malignancy. The physical examination
was unremarkable. Laboratory investigations were within normal
limits except a small thrombocytopenia (PLT 120 000/ul) and
hyperhomocysteinemia (heterozygous MTFHRvariant).
Results:
Doppler ultrasound revealed normal liver size and echo
texture, normal flows and no evidence of collaterals. A TC showed
varicose ectasia in the submucosa on the anterior side of the sigma
until the distal descending colon, the rectum-anal passage and
even in the jejunal-ileal tract in absence of stenosis. A selective
angiography of mesenteric artery exhibited a normal enhancement
in arterial phase while the venus phase confirmed stasis of the
contrast medium from the upper rectum into the terminal ileum,
no evidence of portal venous obstruction. Although no hepatic
involvement was suspected after clinical examination, other
laboratory tests for identifying liver diseases were ordered, an
elastography/liver biopsy resulted normal; a portogram revealed
normal flow and superior mesenteric artery.
Conclusions:
We discussed if submit the patient to a preventive
colonic resection, both considering the elevated hemorrhagic risk
and the neoplastic familiar attitude or to a conservative strategy
with oral therapy. After collegial discussion, we decided for the
second option, propranolol was started at 20 mg bid and tirated
to 40 mg bid over three weeks. After 6 months a new endoscopy
was performed and for the first time of the patient history it was
complete until the ileo-cecal valve which appeared recovered by
adenomatous mucosa (histology: tubular adenoma with dysplasia)
and a polyp was found in the ascendant tract.
One year later from the diagnosis of idiopatic ileo colonic varices,
the patient conditions are stable, at the moment, no gastrointestinal
bleeding has occurred.
P.05.4
A RARE CASE OF MIXED ADENO-NEUROENDOCRINE GASTRIC
CARCINOMA (MANEC) ASSOCIATED TO AUTOIMMUNE
METAPLASTIC ATROPHIC GASTRITIS (AMAG)
Zecchini R.*, Azzolini F., Cecinato P., Iori V., De Marco L., Zanelli M.,
Parmeggiani F., Cavina M., Sereni G., Tioli C., Decembrino F.,
Sassatelli R.
Arcispedale Santa Maria Nuova, Reggio Emilia, Italy
Background and aim:
AMAG is characterised by body and fundus
atrophy, antral preservation and positive antiparietal cell antibody as
result of parietal cells destruction and acid/intrinsic factor reduction.
Gastrin stimulates parietal cells and enterochromaffine-like cells to
proliferate and secrete more acid and histamine, leading to hypo/
achlorhydria, and pernicious anemia. Patients with AMAG have up
to 3–6 fold increased risk of developing gastro-intestinal squamous
tumors and adenocarcinomas (ADK), in addition to neuroendocrine
tumors (NET). Mixed adenoneuroendocrine carcinoma (MANEC) is
a rare condition in which ADK and NET cells coexist for at least 30%
each.
Material and methods:
A 76 years old man with AMAG showed
a 3 cm sessile lesion of the gastric body. The biopsy showed
tubulovillous adenoma with high grade dysplasia associated with
superficial. Helicobacter pylori was negative. AFP, CEA, CA 19-9,
cytokeratin-19 fragment, and 5-hydroxy indoleacetic were normal.
EUS showed suspect of slight submucosal infiltration, CT scan
and PET-CT were negative for metastasis, Endoscopic submucosal
dissection was scheduled.
Results:
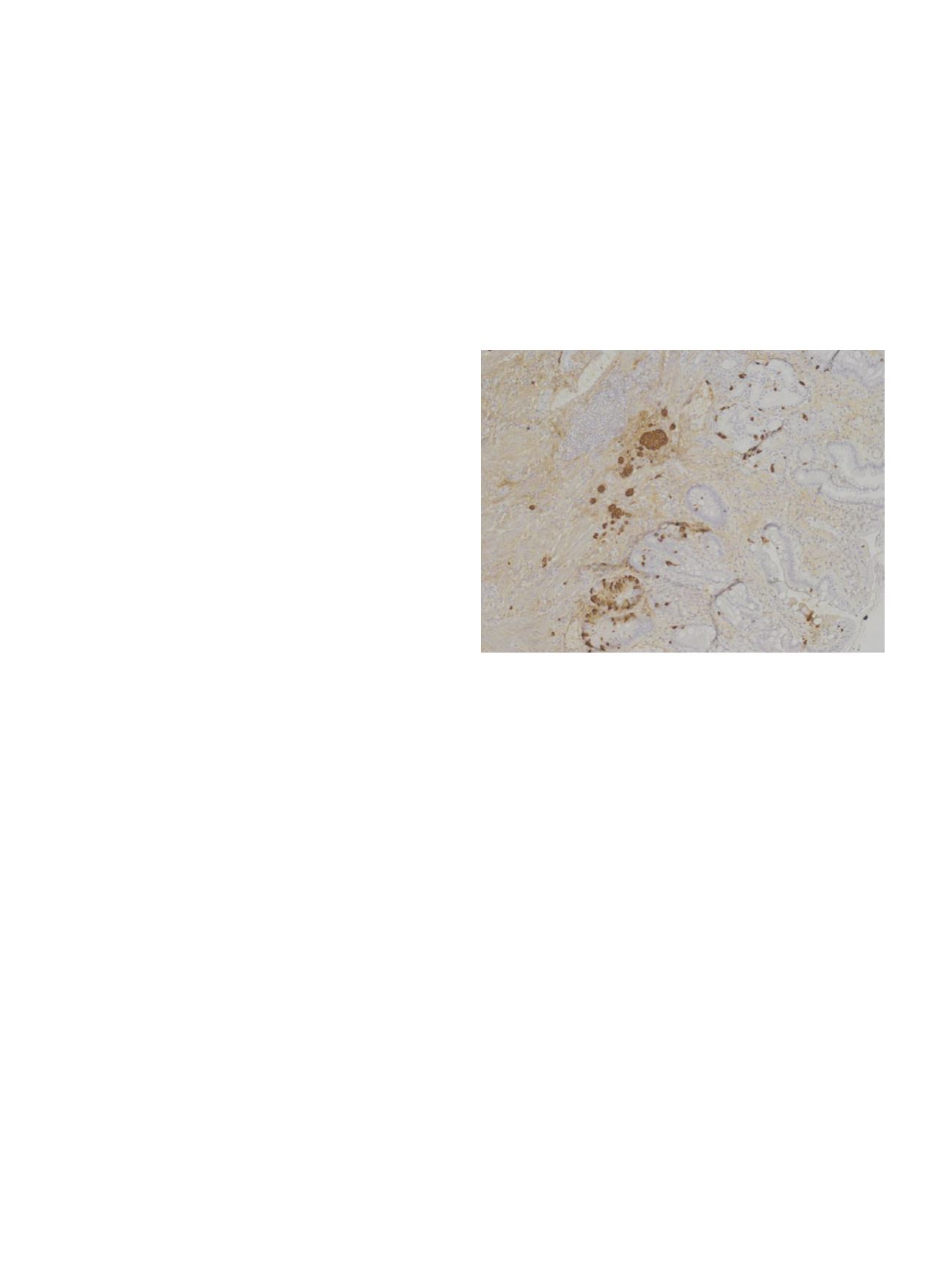
Histological examination revealed poorly differenziated
ADK deeply invading the submucosa with high grade budding, no
vascular invasion and small cell neuroendocrine carcinoma (SC-
NEC). The latter was positive for pancheratin, chromogranin A,
synaptophysin, CDX2, and negative for TTF1.Ki67 labeling index was
60%. As the NEC component was more than 30%, diagnosis of MANEC
was posed.
Subsequently total gastrectomy was performed showing complete
tumor removal and one metastatic glandular lymph node positive
over 29. Tumor was pT1bN1M0, stage IB according to the 7th TNM
calssification. Any chemiotherapy was prescribed for age and
comorbility. The patient is alive without signs of recurrence after 8
months.
Conclusions:
AMAG has an increased risk of cancer development.
The pathway is still unclear. The 2most validated hypotheses suggest:
ADK cells dedifferentiate to NET cells during tumor progression
or monoclonal pluripotent epithelial stem cells differentiate into
2 components. In case of AMAG, mixed lesion must be suspected.
Boost endoscopic survelliance in patients with AMAG possibly with
the help of HD endoscopy must be taken in account in order to
improve their management.
P.05.5
AN UNUSUAL CASE OF DYSPHAGIA
De Filippo F.R.*, De Caro V., Borgheresi P., Romano M., Ciacci C.
AOU San Giovanni di Dio e Ruggi d’Aragona, Salerno, Italy
Background and aim:
Dysphagia is a common symptom especially
in elderly. Esophageal dysphagia is caused by both malignant and
benign diseases. A carefully conducted patient history can be of help
to make a proper diagnosis.
Material and methods:
We here describe the case of a 77 year old
woman who was admitted to the hospital because of solid food
dysphagia. She suffered from hypertension and diabetes. The upper
gastrointestinal examination revealed the presence of a severe
stricture of the upper third of the esophagus (Fig. 1) on which
multiple biopsies were taken. A MR scan of the neck revealed a 2-cm
thickened esophagus along the C6-C7 vertebra with stenosis of the
lumen. There were no lesions of the peri-esophageal fat (Fig 2). A
second endoscopic examination with the ultra-slim endoscope was
performed to complete the study of the upper gastrointestinal tract
and was negative for other diseases. Biopsies were negative for
malignancy and for epithelial dysplasia. However, the pathologist


















